IJCRR - 5(6), March, 2013
Pages: 69-75
Date of Publication: 30-Mar-2013
Print Article
Download XML Download PDF
TUBERCULOSIS DIAGNOSIS AND TREATMENT: NEGOTIATING THE SOLUTION AND IMPLEMENTATIONS
Author: Navjot Kaur, S.S. Bhatia
Category: Healthcare
Abstract:Tuberculosis (TB) is a pulmonary disease caused by Mycobacterium tuberculosis. Various factors are associated with the transmission of TB including the infectiousness of the patient, duration of exposure and the nature of the environment, where exposure occurs. Tuberculosis diagnosis is the key concern of contemporary health research worldwide. TB control has been achieved in high-income countries but remained a threat for middle and low income countries. Transmission of TB can be reduced by fast diagnosis and complete treatment. Appropriate information of control policies and their adequate implementations are mandatory to achieve the desired results. Lack of awareness, inadequate treatment and fall in appropriate implementation on TB control and prevention programs are prevalent factors which become the barrier to achieve the TB elimination target.
Keywords: Tuberculosis, Diagnosis, Treatment regime.
Full Text:
INTRODUCTION
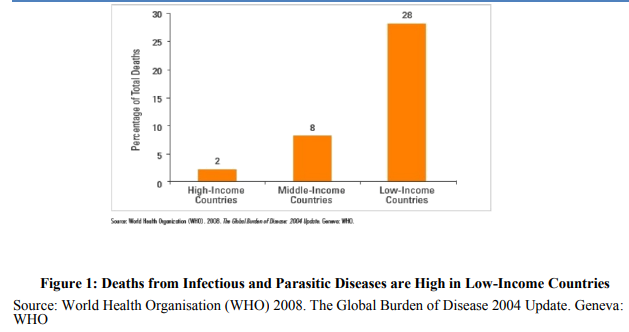
The emergence and re-emergence of bacterial diseases (such as Cholera, Gonorrhea and Tuberculosis) are the main strain for the third world countries. The emergence and persistence of an infectious disease in population becomes the obstacle for economic as well as social development of a nation. The target of Control and Prevention programs is to protect the community and to promote the quality of life. The death rate from infectious and parasitic diseases is approximately 14 times higher in lowincome countries as compare to high-income countries and almost 3 times higher in middleincome countries (Figure 1)1 . Moreover the core factors, which directly affect the transmission of infections, are lack of awareness, migration, urbanization, increased population densities and unhealthy living conditions in urban slums. And the situation becomes troublesome when transmission of infection is uncontrolled because of mismanagement of available drugs which may lead to the re-emergence of the infection.
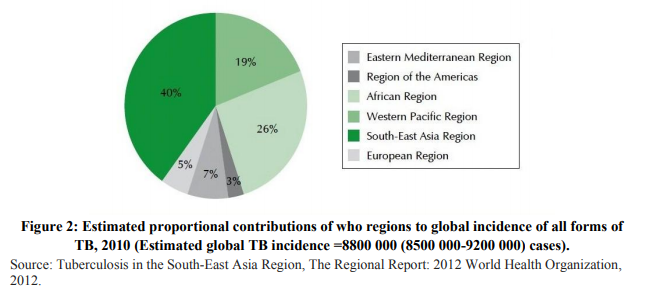
Robert Koch, a German physician, in 1882, has first discovered that tuberculosis is a bacterial infection caused by My-cobacterium tuberculosis, which most commonly affects the lungs but it can also affect other parts of the body such as brain, kidneys, or spine. It transmits from person to person via droplets from the throat and lungs of people with the active TB disease. A person become infective when he/she inhale only a small number of bacteria but infected doesn’t necessarily mean to be sick. It could take years for developing tuberculosis; this stage is called latent TB ( stage in which person carries TB bacteria within body but he/she is not infectious) and can develop active TB disease when their immune system becomes weak by some another reason, such as advancing age, infection with HIV, or some other health problem. 24 March is commemorated as World Tuberculosis Day. It is a day which provides opportunity to raise awareness about the global TB burden and to promote prevention and control efforts, but the question about its complete recovery and elimination is still riddled with multiple problems, which needs strong social and political commitments. The greatest challenge, for health experts, researchers and medical practitioners, is how to overcome the spread of tuberculosis. As per WHO data in 2011, 9 million people are infected with TB and 1.4 million died from this disease and more than 95% of TB deaths are associated with low and middleincome countries. Tuberculosis has been declared as notifiable disease in many countries including India. As per WHO report, geographically the burden of TB is highest in Asia and Africa (Figure 2)2 . Two countries, India and China together account for almost 40% of the world’s TB cases [1].
TREATMENT REGIME AND INADEQUACY
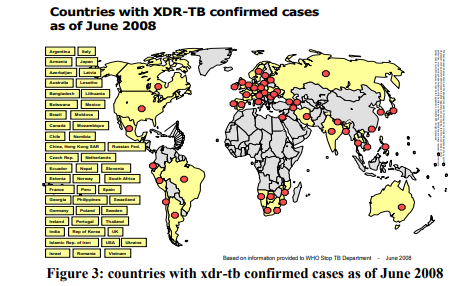
Tuberculosis treatment is based on a combination of antibiotics which is recommended to be taken for half a year or more. But the patients often quit therapy prematurely which increases the risk of drug-resistant strains. The initial phase of TB disease treatment continues for two months and continuation phase usually lasts for four to six month of duration. In the initial phase all patients receive an internationally accepted first-line treatment regimen which consists of isoniazid, rifampicin, pyrazinamide and ethambutol, for two months. The preferred continuation phase consists of isoniazid and rifampicin to be given for four months. Isoniazid and rifampicin are the most powerful bacterial drugs which are active against all populations of TB bacilli [10]. Multidrug-resistant TB (MDR-TB) is a result of mismanagement or failure of the first-line drugs. MDR-TB can be treated with second-line drugs and it takes long time for treatment. There was an estimated 310,000 (range, 220,000-400,000) MDR-TB cases among notified TB patients with pulmonary TB in 2011. Almost 60% of these cases were in India, China and the Russian Federation [1]. In 2005, the extensively drugresistant tuberculosis (XDR-TB) was first reported and identified worldwide [16, 17]. XDRTB is associated with mismanagement of treatment and especially among the individuals co-infected with HIV [21, 22]. XDR-TB strains are created when Multidrug resistant TB (MDRTB) is inadequately treated which actually enables amplification of second-line drug resistance [24, 25]. The treatment options are seriously limited for XDR-TB as it is resistant to first- and second-line drugs. In many of the countries, the actual scale of XDR-TB is unknown due to lack of necessary equipment and the incapability to diagnose it properly.
In June 2008, there were 49 countries which confirmed the cases of XDR-TB [18] (Figure 3). On the basis of data WHO estimates that around 40,000 XDR-TB cases emerges per year. At this stage, Drug-susceptibility testing (DST) for firstline and second-line TB drugs is essentially required for developing effective MDR-TB and XDR-TB treatment regimens. The countries with high incidence of TB, requires laboratory facilities for DST but unfortunately these facilities are not available [17].
REASSESS THE IMPLEMENTATIONS OF DIAGONOSIS
Initiatives are being taken for strengthening the health systems and to promote the use of International Standards for TB Control and Care [15, 29]. TB cases are being reduced with the implementation of Directly Observed Treatment Short-course (DOTS), worldwide. This program was conducted by the British Medical Research Council [8] and the US Public Health Service. World Bank identifies DOTS as one of the most cost-effective available health strategies. From 1995 to 2009, nearly 49 million persons were treated with the implementation of DOTS strategy and 41 million were cured from TB [20]. Technical advisory bodies, WHO and the Global Stop TB partnership, endorse the DOTS strategy to promulgate it globally. Widespread implementation for DOTS has been recently recommended by resources from government(s); the Global Fund for AIDS, Tuberculosis, and Malaria; and the Presidents Emergency Plan for AIDS Relief [12, 13]. DOTS strategy is one of the most successful Stop TB strategies which contains five basic components: i) political commitment with adequate and sustained financing; ii) early case detection and diagnosis through quality-assured bacteriology; iii) standardized treatment with supervision and patient support; iv) effective drug supply and management; and v) monitor and evaluate performance and impact. The DOTS strategy is now confronting other obstacles that are: addressing the risk of HIV, diabetes and multidrug-resistant and extensively drug-resistant TB. Other risk factors which accelerate progression of TB disease include malnutrition, alcoholism, smoking, indoor air pollution in poorly ventilated households and outdoor air pollution at workplace [26]. Earlier M. tuberculosis was exclusively detected by culture which takes weeks because the requisite generation time of 18 to 24 hours. But in low resource settings, diagnosis is done on the basis of smear microscopy as culture may not be available there, and ultimately it leads to the failure in detection of nearly half of TB patients [15]. Recently a molecular diagnostic test, Xpert TB/RIF, is made available for the simultaneous detection of TB and rifampicin resistance directly from sputum within two hours hence is quite simple, rapid and accurate [23]. The technology is based on the GeneXpert platform and is developed as a partnership between the Foundation for Innovative New Diagnostics (FIND), Cepheid Inc. and the University of Medicine and Dentistry of New Jersey, along with support from the US National Institutes of Health [28]. Again cost remains an issue for lowincome countries regarding the adoption of TBXpert project. TB is leading infectious disease which results into death among adults. This situation arises because of the unavailability and inaccessibility of diagnostic tests, which are not adequately implemented. Globally, 37% of TB cases remain undetected, and many of the infectives are not receiving optimal treatment regimens. According to an Indian analysis it has been reported that around 72% of TB patients, who have low living standards (e.g., earning US $1-$2; considered to be in international poverty line), initially look for private health providers before starting the treatment with Revised National TB Program [27]. Apart from all the interventions there is a need to make a check over the problems that are associated with gender, expenditure and availability as well as accessibility of drugs. Here accessibility means that the treatment is not approachable for everyone and everywhere. More over awareness programs associated with transmission and cure of TB should be promoted by mass media.
CONCLUSION
There are number of initiatives which must be implemented to achieve the targeted public health responses: First, accurate measures of the incidence, prevalence, and determinants of TB are required. Second, proper management of TB control program are required to figure out accurate number of TB infectives. Finally, the drugs and treatment must be made available to the infectives via expert medical practitioners. Detecting the infectives and their treatment is challenging enough, but the situation becomes panic due to persistence of drug resistant patients. Eradication of TB is possible only when each TB infective will be detected and treated adequately. As mentioned above TB is a notifiable disease that means each TB case will have to be notified to public health authorities to ensure complete assessment and appropriate treatment and identification of secondary cases. Attention to fundamental aspects of TB control (surveillance, prompt culture and DST, DOTS, contact scrutiny and infection control) is needed to control the spread of TB worldwide. In concluding words we can say that TB can be eradicated from the globe through TB infection control measures including early diagnosis and vigilant treatment of the infectious cases.
ACKNOWLEDGEMENT
The first author Navjot Kaur, would like to express her deep gratitude to Dr. Mini Ghosh for her encouragement and useful suggestions. Authors acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.
References:
1. World Health Organization. Global Tuberculosis Report 2012. http://who.int/tb/publications/global report/gtbr12 main.pdf
2. Centers for Disease Control and Prevention. Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs worldwide. MMWR Morb Mortal Wkly Rep 2006; 55: 301-305.
3. Koch R. Die Aetiologie der Tuberculose: Berliner Klinische Wochenschrift 1882;19:22130. Pinner B, Pinner M, translators. Am Rev Tuberc. 1932; 25:298323.
4. The World Bank. Country and Lending Groups. http://data.worldbank.org/about/countryclassifications/country-and-lending-groups
5. World Health Organization. Global tuberculosis control: a short update to the 2009 report. http://whqlibdoc.who.int/publications/2009/9 789241598866 eng.pdf
6. Fox W. Realistic chemotherapeutic policies for tuberculosis in the developing countries. BMJ. 1964;1:13542.
7. Fendall NR. Auxiliaries and primary medical care. Bull N Y Acad Med. 1972;48:1291300.
8. Fox W. Pillip Ellman Lecture: The modern management and therapy of pulmonary tuberculosis. Proc R Soc Med. 1977; 70:415.
9. Mount FW, Ferebee SH. United States Public Health Service Cooperative investigation of antimicrobial therapy of tuberculosis. V: report on thirty-two week observations on combinations of isoniazid, streptomycin, and para-amino salicylic acid. Am Rev Tuberc. 1954;70:5216.
10. World Health Organization. Treatment of tuberculosis. Guidelines for national programmes. Geneva: World Health Organization, 2003. 11. Rouillon A. The mutual assistance programme of the IUATLD. Development, contribution, and significance. Bull Int Union Tuberc Lung Dis. 1991;66:15972.
12. Raviglione MC, Uplekar M. WHOs new Stop TB strategy. Lancet. 2006; 367:9525.
13. [13] Coggin WL, Ryan CA, Holmes CB. Role of the US Presidents emergency plan for AIDS relief in responding to tuberculosis and HIV coinfection. Clin Infect Dis. 2010;50 (Suppl 3):S2559.
14. Laxminarayan R, Klein EY, Adeyi O. Global investments in TB control: economic benefits. Health A (Millwood). 2009; 28:w73042.
15. World Health Organization. The global plan to stop TB 20112015: transforming The fight Towards The elimination of tuberculosis http://www.stoptb.org/assets/documents/gl obal/plan/TB GlobalPlanToStopTB2011- 2015.pdf
16. Shah N, Wright A, Bai G, Barrera L, Boulahbal F, Martan-Casabona N, Worldwide emergence of extensively drugresistant tuberculosis. Emerg Infect Dis. 2007;13:3807.
17. World Health Organization. Multidrug and extensively drug-resistant TB (M/XDR-TB): 2010 global report on surveillance and response. Report no. WHO/HTM/TB/2010.3. Geneva: The Organization; 2010
18. World Health Organization (2008). Countries with XDR-TB confirmed cases as of June 2008.
19. Centers for Disease Control and Prevention. Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs worldwide. MMWR Morb Mortal Wkly Rep 2006; 55: 301-305.
20. World Health Organization. Global Tuberculosis control 2010. http://whqlibdoc.who.int/publications/2010 /9789241564069 eng.pdf
21. Gandhi NR, Shah NS, Andrews JR, Vella V, Moll AP, Scott M, HIV coinfection in multidrug- and extensively drug-resistant tuberculosis results in high early mortality. Am J Respir Crit Care Med. 2010; 181:806.
22. Gandhi NR, Moll A, Sturm AW, Pawinski R, Govender T, Lalloo U, Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006; 368:157580.
23. Boehme CC, Nabeta P, Hillemann D, Nicol MP, Shenai S, Krapp F, Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010; 363:100515.
24. Cox HS, Sibilia K, Feuerriegel S, Kalon S, Polonsky J, Khamraev AK, Emergence of extensive drug resistance during treatment for multidrug-resistant tuberculosis. N Engl J Med. 2008; 359:2398400.
25. Calver AD, Falmer AA, Murray M, Strauss OJ, Streicher EM, Hanekom M, Emer-gence of increased resistance and extensively drug-resistant tuberculosis despite treat-ment adherence, South Africa. Emerg Infect Dis. 2010;16:26471.
26. Lnnroth K, Castro KG, Chakayah JM, Chauhan LS, Floyd K, Glaziou P, Tuberculosis control and elimination 201050: cure, care, and social development. Lancet. 2010;375:181429.
27. Pantoja A, Floyd K, Unnikrishnan KP, Jitendra R, Padma MR, Lal SS, Economic evaluation of publicprivate mix for tuberculosis care and control, India. Part I. Socio-economic pro le and costs among tuberculosis patients. Int J Tuberc Lung Dis. 2009;13:698704.
28. World Health Organization. http://who.int/tb/laboratory/mtbrifrollout/en/.
29. Hopewell PC, Pai M, Maher D, Uplekar M, Raviglione MC. International standards for tuberculosis care. Lancet Infect Dis. 2006; 6:71025.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License