IJCRR - 5(4), February, 2013
Pages: 103-113
Date of Publication: 28-Feb-2013
Print Article
Download XML Download PDF
SEXUAL BEHAVIORS AMONG HIV PATIENTS ATTENDING ART CENTRE, TERTIARY CARE HOSPITAL, KARNATAKA, INDIA
Author: Ramesh K., Sangeetha Gandhi, Vishwas Rao
Category: Healthcare
Abstract:Introduction: AIDS is a pandemic now. It has multiple risk factors and of all the risk factors, sexual behaviour acts as a double edged sword. On one hand, the risk of HIV acquisition is known to be closely associated with unprotected sexual intercourse and on the other, diagnosis of AIDS is shown to have a paramount importance on the sexual behaviour of the person. Research shows that there are HIV infected people who do engage in unprotected sex, just as there are HIV negative people or people with unknown serostatus who do so. Sex is an integral part of one's living. As we extend our vision to the effects of sexual behaviour following diagnosis of AIDS from conventional view of sexual behaviour as a risk factor, other curious questions take wings. How exactly does diagnosis of AIDS have its influence on sexual behaviour of the diseased? Does the diagnosis of HIV positive help in reducing the risky sexual behaviour or do people still opt to continue the same way? In this study we have tried to discover answers to some of these questions. Materials and Methods: A case-series study was conducted among HIV positive patients coming to the ART centre for seeking treatment at ART Centre,Vijayanagara Institute of Medical Sciences Bellary, Karnataka from Novmber 2011 to April 2012. The sample size of the study is 400 and non probability sampling technique was used. Permission from respective authorities and written consent from study participants was obtained. Data was collected using a pre tested semi structured questionnaire. Data was analyzed using SPSS 15.0 and McNemar test was used to compare qualitative variables before and after diagnosis of AIDS. Results: The study subjects included both males (54%) and females (46%). The educational status is less than primary schooling in 88% of study subjects and 90% are married. Among patients, 48% were diagnosed on routine blood investigation and 40% on voluntary. There is no much difference in use of contraceptives before (16%) and after (18%) diagnosis but there is a significant difference in Condom use (before- 20% and after-37%). Sex with multiple partners was found in 34% of patients before diagnosis but it reduced to 13% after the diagnosis. There is no change in alcoholic behaviour. Even after diagnosis, 33% patients continued have unprotected sex with their partners and 25% of patients lost interest in sex after diagnosis. Conclusion: Even after the diagnosis, many sexual risk behaviours remain unchanged among HIV positive patients.
Keywords: Hiv, ART, Mode of transmission
Full Text:
INTRODUCTION
India has an estimated 2.4 million people living with HIV1 . The HIV epidemic is highly heterogeneous, and the majority of HIV infections occur through heterosexual transmission, with unprotected sex, particularly in the southern states2 . There is little published evidence demonstrating the efficacy of female sex worker (FSW) preventive interventions, either in India3,4 or elsewhere5 .Nowadays, interventions to stem the spread of the Human immunodeficiency virus (HIV) throughout the world are as varied as the contexts in which we find them. HIV epidemic dynamic can be curtailed by not only preventive and treatment options, but also by in depth study of sexual Behavior. This pattern of sexual behavior is widely diverse and influenced by society, culture, custom and tradition. Understanding these factors influencing sexual behavior plays vital role in formulating strategies to combat HIV spread. The predominant mode of HIV infection throughout SouthAfrica is unprotected heterosexual intercourse6 . Prevention programs that target secondary transmission between those known to be HIV positive and their sexual partner have recently gained favor7 but are still underdeveloped in general epidemic setting8,9,10 . Better understanding of patterns of sexual behavior among individuals who know their HIV status remains centered to these efforts11 . Knowledge about unsafe sexual behavior of HIV infected individuals is therefore, crucial for development of specific intervention to reduce sexual transmission12. Progress to promote safer sexual behavior is effective and should be widely disseminated. Here we present the findings of behavior changes of HIV positive patients. This provides insights into the potential prevention benefits in future.
METHODOLOGY
A descriptive case series study was conducted among HIV positive patients coming to the ART centre for seeking treatment at ART Centre, a tertiary care hospital, Bellary, Karnataka from November 2011 to April 2012. Totally 10,000 patients have registered and among them 5000 patients were on treatment at ART centre. Hence the sampling frame included those patients who were on treatment. Totally 400 patients were included for the study. These 400 patients were selected based on non probability purposive sampling technique. Data was collected using a semi structured questionnaire which contained information regarding socio demographic details and behavior. Written informed consent was taken and by interviewing patients, data was collected. After the data collection, health education was given to study subjects on Prevention and treatment of HIV. This study excluded those Patients who were seriously ill and who did not give consent. Data was entered in Microsoft excel and analyzed in SPSS 15. The statistical tests used were Proportion, Mean, Standard deviation, Mcnemar test and Wilcoxon sign rank test.
RESULTS
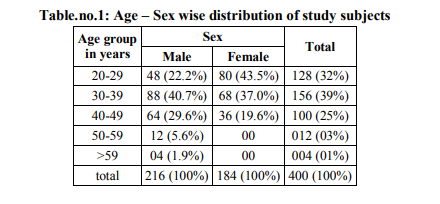
Out of the 400 subjects in our study 216 were males (54%) and 184 were females (46%). Out of the 216 male subjects, 40% of them were between the age of 30-39 yrs, 29.6% were in the age group of 40 – 49 years, 22.2% were between the age group of 20-29, 5.6% were between age group 50-59 and only 1.9%. Among the female subjects, unlike the male subjects in whom majority were in age group 30-39 years of age, majority were in between the age groups of 20- 29 years. Out of the 184 female subjects, 43.5% were in between the age group of 20-29 yrs. 37% were in the age group of 30-39 years, and 19.6% were in between the age group of 40-49 yrs.
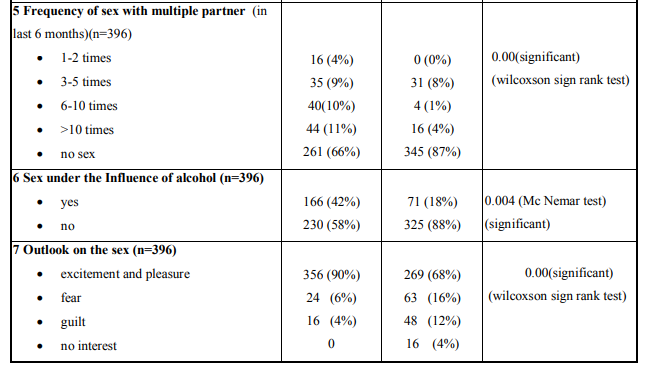
Education
Out the 400 subjects taken for our study, 45% of them were illiterates, 43% had just primary education, 9% subjects had high school education and only 2% of them had completed their education till pre university level (Fig.1).
Occupation
In our study about half of the study subjects were unskilled workers primarily daily wage workers followed by semi skilled and skilled workers who formed 22% and 19% respectively;49 % were unskilled; 7% were professionals (Fig.1).
Marital status
Marital status of the patient was known to generally access the sexual behavior among the subjects. Those who are unmarried are assumed to have Pre marital sex whereas those who are married are assumed to either have sex with either their wives or indulge in extra marital sex. In our study it was found that only 10% of the HIV positive subjects are unmarried (Fig.1).
Income
Poverty is root cause of all the evil in India including the high rates of HIV. Among our study subjects 62% of them earned an income of about 3000-6000Rs per month.17% of them earned an income less than 3000 Rs per month; 21% of them earned an income of more than 6000 Rs per month (Fig.1).
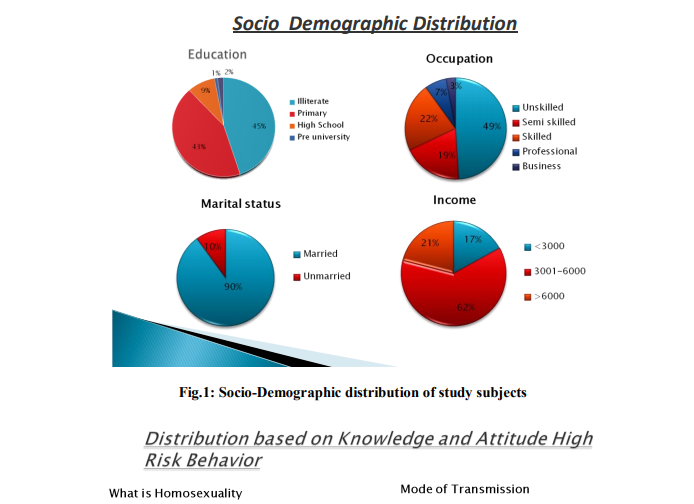
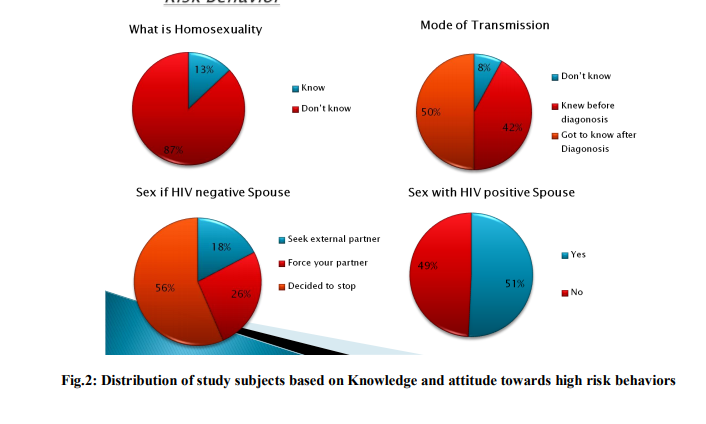
Homosexuality
Homosexuality is the major mode of transmission of HIV in Western countries but in India the major mode of sexual transmission is among heterosexuals. This was also confirmed in our study in which 87% of the study subjects were ignorant to the concept of Homosexuality and did not know what it was. (Fig.2)
Mode of transmission
Poverty and Illiteracy are both very high in India. This has led to ignorance and lack of knowledge among the people in Indian society towards the mode of spread and prevention of HIV, It was seen that about half of our study subjects (50%) got to know about the mode of spread of infection only after their diagnosis and 8% did not know the mode of transmission even after diagnosis. (Fig.2)
Sex with HIV negative spouse
In our study we tried to find out the change in the sexual behavior among subjects whose spouse were not affected with HIV (n=215) and it was found that majority of the people, 56% of study subjects have stopped having sexual intercourse completely whereas 18% of study subjects seek external partner for sex and whereas 26% of the subjects continue to have sex with their spouses. (Fig.2)
Sex with HIV positive spouse
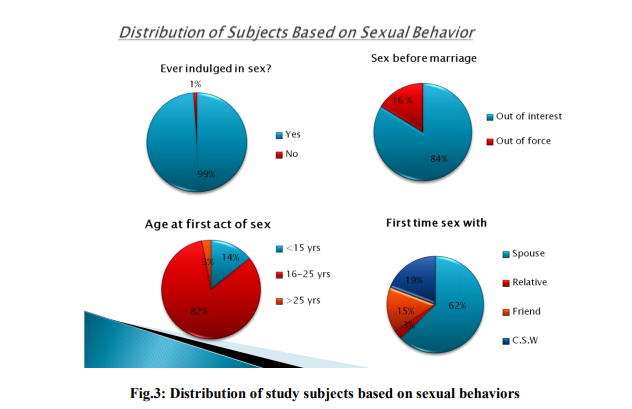
In our study we also tried to find the Sexual behavior among study subjects whose spouse were affected with HIV(n=185) and it was found that half of the study subjects had no change in sexual behavior and continued to have sex with their partners whereas the other half stopped having sex with their infected partner. (Fig.2) Among our study subjects, 99% of the subjects confessed they had indulged in a sexual intercourse at least once. (Fig.3)
Sex before marriage
In our study out of the 396 study subjects who had intercourse at least once, 110(27.7%) of them had sexual intercourse before marriage. And among those who had sex before marriage, 84% of them had intercourse out of their own interest whereas sizeable number of the study subjects (16%) was forced (Fig.3).
Age at first act of sex
Among 396 study subjects who confessed that they had indulged in a sexual intercourse at least once, 82% of the subjects had first act of sexual intercourse between 16 to 25 years age group; 14% had below age of 15 years and 3% had above age of 25 years (Fig.3).
First time sex with
In our study, Out of the 396 study subjects, 62% of the study subjects had their first sexual encounter with their spouse. Sizeable numbers of the study subjects have had their first sexual encounter with a Commercial Sex Worker (19%) and the rest with either friend or relative. (Fig.3) We next asked the participants of our study regarding the various sexual behaviors they might have participated in and if they do so after diagnosis.
Frequency of sex
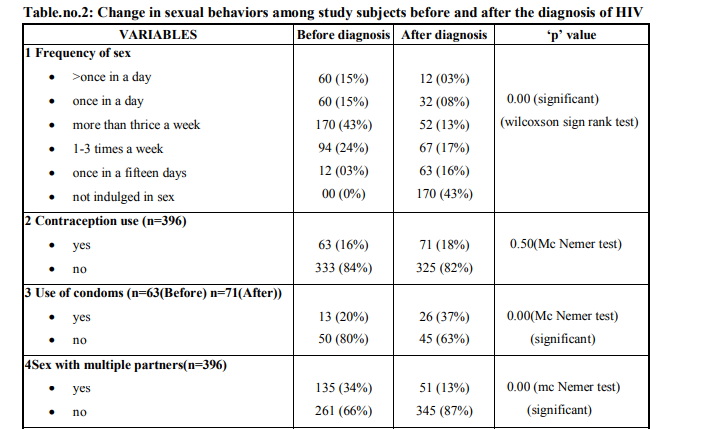
When asked about frequency of sex of the patient in the 6 months before diagnosis , nearly half (43% of the study population) of the respondents reported a frequency of 3 times a week, 24% of the respondents reported about 1- 3 times a week with none reporting abstinence from sex. In comparison, 43% reported abstinence from coitus and 17% respondents reported having sex 1-3 times a week for the past 6 months after diagnosis. There is a significant decrease in the frequency of sex after diagnosis of HIV. (Table.no.2)
Use of condoms
When we asked the respondents about their condom use in the 6 months before diagnosis an overwhelmingly large number of study subjects (80%) reported not using condom before coitus and only 20% of study subjects reported using condoms. In comparison, 37% reported using condoms in the 6 months after diagnosis and 63% respondents did not use condoms in the 6 months after diagnosis. There is a significant increase in the condom use among the HIV patients in the 6 months after diagnosis according to. (Table.no.2)
Sex with multiple partners and frequency
We then enquired with the study subjects if they engaged in sexual activity with multiple sexual partners (MSP) and if yes, what was the frequency of sexual activity with multiple sexual partners. Of the 396 study subjects 135(34%) subjects told that they did engage in sex with multiple sexual partners in the 6 months before diagnosis of HIV. Out of the 135 subjects who engaged in sex with MSP, 66% had sex with more than 10 partners, 11% with about 6-10 partners in the 6 months before diagnosis. In comparison, after diagnosis of HIV, out of the same 396 study subjects only 13% told that they did engage in sexual activity. (Table.no.2)
Alcohol consumption
We asked our study subjects about their alcohol consumption and regarding the High risk practice of sex under the influence alcohol. Out of the study subjects who consumed alcohol, 42% of the subjects reported having sex under the influence of alcohol. This value reduced after diagnosis, when only 18% of subjects reported having sex under the influence of alcohol. (Table.no.2)
Outlook on sex
The final finding of our report is the gross change in the perception and attitude of the subjects towards sex. Before the diagnosis of HIV, 90% of the subjects approached sex with excitement only 10% reporting approach to sex with fear and guilt. This outlook has drastically changed post diagnosis where only 68% of subjects approached sex with excitement. While 16% associated fear with sex, and the other 12% of subjects associated sex with guilt. (Table.no.2) So change in sexual behavior related to frequency of sex, use of condoms, sex with multiple partners, sex under the influence of alcohol, and outlook on sex were found statistically significant before and after the diagnosis.
DISCUSSION
In our study out of the 400 subjects, 54% were male subjects and 46% were female subjects. On a total, high proportion of subjects fell between age group 30-39 years. Similar findings were observed in a study conducted in India in which 41% were female subjects and 59% were male subjects; majority of them fell between age groups 30-34 years13. In another study as well maximum subjects fell between age group 35-49 years14 . Illiteracy is one of the major reasons for the rampant increase in the number of HIV positive cases. Out of the 400 subjects taken for our study, 45% of them were illiterates. Compared to the similar study done, 30% were illiterate; 24% had a primary education; 36% had a high school education and 10% had a higher education; whereas in our study there were significantly more number of illiterates and less number of subjects with pre-university education13 .
Compared to another similar study done in south India, 25% were illiterate; 50% were educated till high school; 25% were educated up to predegree, but in our study there were significantly more number of illiterates and less number of subjects with high school and pre-university education15. In our study, about half of the study subjects were unskilled workers primarily daily wage workers followed by semi skilled and skilled workers. Compared to a study in INDIA, 19% were unemployed; 81% were employed13 . Compared to another study done in Goa, 66.3% were employed, 15.7% were unemployed and 18% are students16. Whereas in our study, we have a larger unemployed population. Poverty is root cause of all the evil in India including the high rates of HIV. In this study, a maximum number of study subjects earned an income of about 3000-6000 rupees per month (62%). Compared to a similar study, 15% are poorest; 15% were poorer; 3% were middle class; 32% were rich; 15% were richest13; whereas in our study 17% have a very low income and there is no question about rich or richest in our study. Compared to other study, 16% had a low standard of living index; 32% had a medium standard of living indexand 52% had a high standard of living index17 . Marital status of the patient was known to generally access the sexual behavior among the subjects. In our study, it was found that only 10%of the HIV positive subjects are unmarried therefore it can be assumed that the pre marital sex leading to HIV is quite low. Compared to a study done in Chennai 55% are married; 35% were single; 7% were separated; 2% were divorced18. Whereas in our study a significant large number of them are married. In India, the major mode of sexual transmission is among heterosexuals. But when asked about homosexuality, 87% of the study subjects were ignorant to the concept of Homosexuality and did not know what it was. The finding is similar to a study by moni nag19 . It was seen that about half of our study subjects got to know about the mode of spread of infection only after their diagnosis and some did not know the mode of transmission even after diagnosis. Compared to a similar study by Coates TJ et al20, 40% men andwomen knew the exact mode of transmission of HIV, the findings match with our study. Compared to a similar study done in pune21 , Nearly one-third of the men had never heard of AIDS at their screening visit, and less than 25% were able to correctly answer more than nine out of 12 questions on modes of HIV transmission.the findings match with our study. Compared to a study done in uganda22, 9% of male study subjects had unprotected sex with negative partner (forced) and 5% of female study subjects had unprotected sex with negative partner (forced).whereas in our study there were significantly large number who forced their partner. Compared to a similar study23 in India, 89% male subjects were HIV positive andforced their wife for intercourse and 19% female subjects were HIV positive andforced their husband for intercourse. Whereas in our study the number is not that high, the majority stopped sexual intercourse. Among our study subjects, 99% of the study subjects confessed they had indulged in a sexual intercourse at least once. . Late adolescent age group is at threat age group; teenage pregnancies are slowly rising as well. Out of 495 subjects, 14% of the subjects had first act of sexual intercourse before 15 years of age. Compared to a similar study 20, about 12% of study subjects had sexual intercourse before 15 years of age, the findings match with our study. The major Sexual changes are brought about in between the husband and wife depending on the sero status individually. These changes may be attributable to the emotional turmoil in a person infected with HIV or may be due to apprehension of the person towards sex or due to fear of infecting their HIV negative spouse.
These changes have both desirable and undesirable effect. For example, a HIV positive individual may refrain from having sex with his wife due to fear of transmitting infection to her , which is a desirable effect but in turn might visit Commercial sex worker (CSW) and create a nidus for further spread of infection. Hence it is imperative to understand the change in sexual behaviour between husband and wife after diagnosis of HIV. In our study we found that 56% abstained from sex with sero negative spouse which is a healthy finding but 26% approached CSW. This shows the importance of counseling of the sero positive patient regarding his or her moral obligation to his/her spouse and social obligation to the society. These steps to ensure decreased transmission are even more important in the first 6 months of diagnosis of HIV as even temporary reduction in high risk sexual activity has shown to help curtail the spread of HIV within highly active sexual networks, given that per-act probability of transmission of infection is high at this stage of disease. In case of infected individual with sero positive spouse, it is safe practice to have a sexual intercourse. But in our study we found that about half the individuals refrained from sex with sero positive spouse. Almost similar results were found in the study conducted in California24. We also found that the frequency with which the sero positive study subjects had sex also had considerable decrease with increase in the number of individual who abstained frome sex. These changes may be due to apprehension of the person towards sex or due to emotional upheaval caused by diagnosis of HIV. It has been established in other studies that women face more emotional and sexual disturbances25 and men report greater sexual satisfaction and decreased sexual difficulties after diagnosis of HIV26. It has also been reported that HAART has been associated with decrease in libido in men due to increased libido.Government and NGO,s need to address this aspect of a sero positive individual to ensure HIV person leads a happy and healthy life. The biggest risk factor for contracting HIV infection and Spreading HIV infection is sexual contact with multiple sexual partners. This trend is seen in young adults and adults alike. One of the major sexual behaviors causing this trend is Pre marital sex and post marital multiple sex partners (MSP). Unlike even a decade ago, pre marital sex is increasing in India27.This trend may be attributed to increased surveillance and research as a part of HIV prevention as well as more relaxed sexual mores noted recently. These behavior may also be facilitated by communication in unmarried men social network that encourages sexual exploration but places more weight on sexual experience than sexual health. There was a considerable decrease in the number of partners and the frequency of sex with MSP after diagnosis of HIV in our study. But emphasis needs to be laid to reduce the number of partners to lead a healthy life. Condom use has been the highlight of the government efforts to prevent the spread of HIV AIDS. Its various initiatives like providing condoms free of cost, aggressive campaigning in print media and TV has had a considerable effect in reducing the HIV infection across country , especially in cities. The acceptance of condom has generally been low in the villages .Various factors like low availability, decreased privacy at the condom provider, cultural barriers have prevented success of the condom. Also the major factor is the lack knowledge among people regarding the efficacy of the condom to reduce HIV prevention. Our study showed a considerable increase in the usage of condoms after the diagnosis of HIV compared to before diagnosis. This shows the change towards healthy sexual attitude of the subject. But the bottom-line is, the change of sexual behavior is too small to be proud of (20% to 37%).Effective strategies need to be developed to improve the usage and acceptability of condoms.
CONCLUSION
HIV positive patients changed their sexual behaviors related to frequency of sex, use of condoms, sex with multiple partners and their outlook on sex significantly after the diagnosis of HIV
References:
1. UNAIDS Asia: AIDS epidemic summary: regional summary. http://data.unaids.org/pub/Report/2008/jc15 27_epibriefs_asia_en.pdf, 2009. (Accessed 7 April 20011).
2. Halli SS, Blanchard J, Satihal DG, et al. Migration and HIV transmission in rural South India: an ethnographic study. Cult Health Sex 2007;9:85–94.
3. Gangopadhyay DN, Chanda M, Sarkar K, et al. Evaluation of sexually transmitted diseases/human immunodeficiency virus intervention programs for sex workers in Calcutta, India. Sex Transm Dis 2005;32:680–4.
4. Fung IC, Guinness L, Vickerman P, et al. Modelling the impact and cost-effectiveness of the HIV intervention programme amongst commercial sex workers in Ahmedabad, Gujarat, India. BMC Public Health 2007;7:195.
5. Foss AM, Hossain M, Vickerman PT, et al. A systematic review of published evidence on intervention impact on condom use in sub-Saharan Africa and Asia. Sex Transm Infect 2007;83:510–16.
6. UNAIDS, WHO. AIDS Epidemic Update. Genera,Switzerland:UNAIDS, WHO;2005
7. Centre for Disease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV : recommendation of CDC, the Health Resources and Services Administration, the National Institute of Health, and the HIV Medicine Association of the Infectious Disease Society of America. MMWR Moch Mortal Wkly Rep. 2003;52(RR-12):1-32.
8. Indyk D, Golub S. The shifting locus of riskreduction: the critical role of HIV infected individuals. Soc Work Health Care2006;42:113-132.
9. Janssen R, HoltgraveD, Valdeserre R, etal. The serostatus approach to fighting the HIV epidemic: prevention strategies for infected individuals. Am J Public Health. 2001;91:1019-1024.
10. Sexual Behavior and Reproductive Health among HIV-Infected patients in Urban and Rural South Africa. J. AIDS 2008;47: 484- 493
11. Prevalence of Unsafe Sexual Behavior Among HIV-Infected Individuals: The Swiss HIV Cohort Study JAIDS Journal of Acquired Immune Deficiency Syndromes 33:494–499 © 2003 Lippincott Williams and Wilkins, Inc., Philadelphia 494
12. NIH Consensus Statement. Interventions to prevent HIV risk behaviours. 1997;15(2):1– 41
13. Perkins JM, Khan KT, Subramanian SV (2009) Patterns and Distribution of HIV among Adult Men and Women in India. PLoS ONE 4(5): e5648. doi:10.1371/journal.pone.0005648
14. Journal of Urban Health: Bulletin of New York Academy of Medicine, Vol-83, No.4.2006
15. Chandra PS, Satyanarayana VA, Satishchandra P, Satish KS, Kumar M. Do men and women with HIV differ in their quality of life? A study from South India. AIDS Behav. 2009 Feb;13(1):110-7. Epub 2008 Jul 25.
16. Vaz FS, Ferreira AM, Kulkarni MS, Motghare DD. Sexual risk behaviors and HIV/AIDS awareness among males in a rural community in Goa. J Commun Dis. 2006 Mar;38(1):74-8.
17. An Lwin, Thein Z., "An Examination of the Association between HIV Related Knowledge, Attitudes, and Behaviors and HIV Infection Status in Five High HIV Prevalence States in India." (2011).PublicHealthTheses. Paper168. http://digitalarchive.gsu.edu/iph_theses/168
18. Solomon SS, Celentano DD, Srikrishnan AK, Vasudevan CK, Anand S, Kumar MS, Solomon S, Lucas GM, Mehta SH. Mortality among injection drug users in Chennai, India (2005-2008). AIDS. 2009 May 15;23(8):997-1004.
19. 19.Moni Nag. Sexual behaviour in India with risk of HIV/AIDS transmission. Health Transition Review, Supplement to Volume 5, 1995, 293-305.
20. Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008 Aug 23;372 (9639):669-84.
21. HIV testing and counseling among men attending sexually transmitted disease clinics in Pune, India: changes in condom use and sexual behavior over AIDS. 1998 oct 1;12(14):1869-77
22. Changes in sexual behavior and risk of HIV transmission after antiretroviral therapy and prevention interventions in rural Uganda AIDS. 2006 jan 2;20(1):85-92
23. HIV transmission in Intimate Partner Relationships in India UNAIDS Nov2009
24. Sexual risk behaviors among heterosexual HIV serodiscordant couples in the era of post-exposure prevention and viral suppressive therapyAIDS. 2000 mar 10;14(4):F47-54.
25. Stall R, Duran L, Wisniewski SR, Friedman MS, Marshal MP, et al. (2009) Running in place: implications of HIV incidence estimates among urban men who have sex with men in the United States and other industrialized countries. AIDS and behavior 13: 615–29. doi:10.1007/s10461-008-9509- 7.
26. Chandra PS, Carey MP, Carey KB, Prasada Rao PS, Jairam KR, Thomas T. HIV risk behaviour among psychiatric inpatients: results from a hospital-wide screening study in southern India. Int J STD AIDS. 2003 Aug;14(8):532-8.
27. Rohit Sharma. More than a quarter of India's youngsters have premarital sex. BMJ 2001(10 March); 322: 575.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License