IJCRR - 5(4), February, 2013
Pages: 85-92
Date of Publication: 28-Feb-2013
Print Article
Download XML Download PDF
PALATO-RADICULAR GROOVE - HIDDEN ROUTE TO DESTRUCTION - CASE REPORT
Author: Maheaswari Rajendran, Kiruthika Sivasankar
Category: Healthcare
Abstract:Aim: To treat cases of palato-radicular groove associated with localised periodontitis using conservative and/or regenerative approach based on the depth and extent of the groove. Objective: To utilise various regenerative approaches in the management of palato-radicular groove with associated periodontitis in order to enhance the regeneration of the lost periodontium. Case description: Three cases of unilateral PRG with localised periodontitis involving the maxillary lateral incisor in 2 cases and central incisor in 1 case has been discussed. The article showcases the result of conservative and /or regenerative approach used in the management of these cases. Bone graft, platelet rich fibrin and guided tissue regeneration using resorbable membrane has been used in the treatment depending on morphology and depth of intrabony defect. Conclusion: Thorough examination by the clinician helps in early detection of palato-radicular groove and prevents the loss of the periodontium. Palato-radicular groove associated with severe localised periodontitis can be successfully managed using various regenerative approaches.
Keywords: Palato-radicular groove, localised periodontitis, guided tissue regeneration, platelet rich fibrin, bone graft.
Full Text:
INTRODUCTION
Developmental anomalies of the maxillary incisors include deformations of crown and root, supernumerary teeth, calcifications of the pulp chamber etc. One such anomaly occurring in the maxillary incisors is Palato-radicular groove (PRG). These grooves are also known as palatogingival groove (1), radicular groove (2) etc. Palato-radicular groove is a developmental, anomalous groove usually found on the palatal aspect of maxillary incisors. (3) They are considered as an infolding of the enamel organ and epithelial sheath of Hertwig. (1) These grooves originate in the crown and terminate in different directions and distances along the root.(4) In a recent study by Albaricci et al 2008(5) reported prevalence of PRG as 11.1% in maxillary lateral incisors. Among them 62.8% of the grooves were proximally located; 57.8% originated form lingual fossa. Most of the grooves had an oblique and tortuous course on the root. PRGs serve as plaque retentive areas which lead to clinical attachment loss and pocket formation. Lee et al first reported the association between PRG and localized periodontitis. (1) Radiographically, the groove is seen as a radiolucent line simulating the root canal of the involved teeth hence is referred to as parapulpal line. (6) But this is not a consistent finding. Management of PRG depends on the depth and the extent of the groove, association with the pulp and presence of intrabony defect. Treating cases of PRG with localized periodontitis involves both the management of the groove and the associated pathology. This article presents a series of case reports successfully managed by different procedures involving periodontal and/or restorative approach.
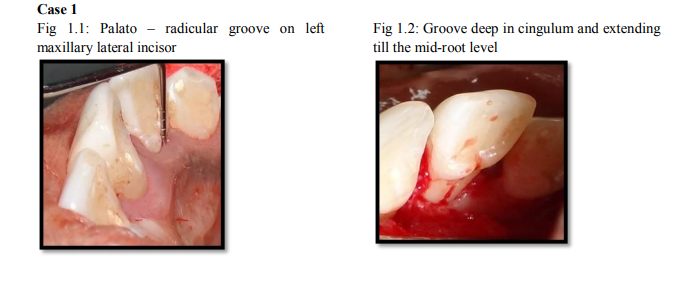
CASE 1
A 21 year old female patient reported to the outpatient department, Department of Periodontics, with a chief complaint of spacing in the upper and lower anteriors. On routine examination an asymptomatic groove was noticed on the mid-palatal aspect of the right maxillary lateral incisor originating in the cingulum and extending apically on the root. On periodontal examination probing depth and clinical attachment level (CAL) of 6mm was present along the groove (Figure 1.1). On testing the vitality, the tooth was found to be vital. Intra-oral periapical radiograph revealed no evidence of parapulpal line or peri-apical pathology. Blood investigation revealed values in normal range. Phase I periodontal therapy consisting of Oral hygiene instructions, Scaling and root planing was performed. During re-evaluation, probing depth was persistent hence periodontal flap surgery was planned. Under LA, envelop flap was elevated on the palatal aspect and PRG was found to be deep in the cingulum and became shallow as it extended till the mid root level (Figure 1.2). After degranulation, the root portion of the groove was managed by saucerisation. Crown portion was restored with Glass Ionomer Cement (GCFuji I, Blackwell supplies, Essex) to normal contour and the flap was approximated and sutured (Figure 1.3). Post surgical instructions were given along with anti-microbial coverage. Patient was reviewed at one month interval for three months to facilitate and encourage oral hygiene maintenance during which no probing was performed. On periodontal examination after 7 months probing depth was reduced to 3mm (Figure 1.4).
CASE 2
A 32 yr old female patient reported to the department of Periodontics with complaint of mobility in relation to right maxillary lateral incisor. On examination, tooth exihibited grade II mobility with probing depth and clinical attachment level of 9mm both labially and palatally (Figure 2.1). A deep palato-radicular groove was present midpalatally extending along the root. Intra-oral periapical radiograph revealed vertical bone loss involving the apical third of the root and periapical pathology (Figure 2.2). The tooth was non-vital. The tooth was temporarily stabilized with braided stainless steel wire and flowable light cure composite for 6-8 weeks and root canal therapy was done. Non- surgical therapy was performed after routine investigations. On reevaluation after 2 months, mobility had reduced to grade I but the probing depth was persistent. Hence periodontal flap surgery was planned. Under LA, full thickness flap was elevated both labially and palatally with vertical releasing incision on the labial aspect. Deep groove was found extending from the cingulum to the apical third of the root. Intra-bony defect was found extending from palatal to labial aspect with dehiscence of the labial cortical plate(Figure 2.3, 2.4). Deep portion of the groove was sealed using GIC (GCFuji I). Demineralised bone matrix xenogeneic graft (Osseograft, Encoll, U. S. A) placed in the defect both labially and palatally (Figure 2.5). Platelet rich fibrin was placed labially covering the dehiscence and flaps were approximated (Figure 2.6). Antibiotics and analgesics were prescribed. Patient was reviewed periodically to examine the oral hygiene maintenance. After nine months the probing depth and CAL was 3mm and 4 mm respectively (Figure 2.7). Mobility was grade I. Post operative radiograph showed evidence of bone fill in the crestal region.
CASE 3
A 23 year old patient referred to the Department of Periodontics, with non vital, rotated and mobile left maxillary central incisor. On examination, mucosal fenestration was present on the labial gingiva with a palato-radicular groove extending along the mesio-palatal aspect of the root with grade II mobility. Probing depth was 10mm mesially and 9mm palatally; CAL was 11mm mesially and 9 mm palatally (Figure 3.1). Midline diastema and extrusion was present. Intra-oral periapical radiograph revealed root canal treated maxillary left central incisor with vertical bone loss on the mesial aspect extending till the apical third of the root (Figure 3.2). Non surgical therapy was performed after routine investigations. Probing depth was 7mm mesio-labially and 6mm palatally on review and surgery was planned. Under LA, muco-periosteal flap was elevated both labially and palatally. Shallow palatoradicular groove extended along the mesiopalatal aspect of the root which terminated in a combined intra-bony defect (Figure 3.3). Radiculoplasty was done with surgical diamond burs. Demineralised bone matrix xenograft was placed in the bony defect and covered with resorbable collagen membrane (Healiguide, Encoll, U. S. A). The membrane was adapted to the tooth using chromic catgut 5-0 suture material (Figure 3.4). Flap was approximated using 3-0 black silk suture material. Periodontal dressing was given with Coe-pack. Patient was reviewed periodically and the healing of the mucosal fenestration on the labial aspect was satisfactory. Nine months post surgery revealed probing depth and CAL of 2mm and 3mm respectively. The tooth was aesthetically corrected by ceramic crown (Figure 3.5). Evidence of bone fill was seen in the defect on the mesial aspect of the tooth radiographically after 9 months (Figure 3.6).
DISCUSSION
Palato-radicular groove (PRG) is a rare developmental anomaly of the maxillary incisor teeth. The association between PRG and localized periodontitis depends on the extent and depth of the groove on the root (1) . PRGs with localized periodontitis usually presents as a perio-endo lesion. These grooves with funnel shaped morphology serve as plaque retentive area and extend along the root. This leads to attachment loss and pulpal necrosis (1) . Channels may be present at the depth of the groove which acts as a passage for the bacterial toxins to gain entry into the pulp canal. (14) Hence most of the cases of PRG with localized periodontitis require endodontic treatment. PRGs may be symptomatic or asymptomatic. Grooves limited to the cingulum usually do not cause damage to the periodontium. Hence these grooves are asymptomatic and intensive treatment is not required. Deep grooves associated with intrabony defect require both periodontal and endodontic management. Parapulpal line observed radiographically is not a pathognomonic feature because these lines are most often obscured by the radiolucent root canal. None of our cases showed these lines radiographically. Recently computerized tomography (CT) has been used in determining the extent of the groove. CT shows the 3D image of the groove and also its proximity with the root canal. (8) Successful management of PRG with localized periodontitis involves two aspects: treating the groove and the resultant pathology (intrabony defects, if present) Prognosis of the tooth with PRG depends on the depth, location and termination on the root. (4) In case 1, the tooth with the groove was asymptomatic. The groove was detected only on routine examination. Crown portion of the groove was deep and was restored with GIC (Fuji I) to normal tooth contour. In case 2, PRG was deep and terminated in an intrabony defect palatally which extended to the labial aspect. Labial cortical plate dehiscence was present. The combination of restorative and surgical approach was done. Different restorative materials have been used in the past which includes amalgam (9), GIC (10, 11) , composite (11) and mineral trioxide aggregate. Glass Ionomer Cement (Fuji I) was used in all the cases due to its property of resistance to water degradation at the tooth – cement interface, sealing ability and good chemical bonding.(10.11) Moreover, studies have reported that during healing epithelial and connective tissue attachment occurs on the cement surface.(12) Various regenerative materials currently used to fill the intra bony defects are bone grafts, platelet rich plasma (13), and enamel matrix derivative (14). In this case, bone defect was filled with demineralised xenograft both labially and palatally. As this bone substitute is osteoconductive, Platelet rich Fibrin (PRF) was placed covering the labial dehiscence. Platelet rich Fibrin belongs to a new generation of platelet concentrate. It is an immune platelet concentrate collecting on a single fibrin membrane all the constituents of a blood sample (cytokines, growth factors etc) for favorable tissue healing. (15) In case 3, as the groove was shallow on the root, radiculoplasty was performed. The defect was a combined intrabony defect with two walled defect on the coronal aspect. Hence bone graft was placed with resorbable membrane covering the osseous defect. Guided tissue regeneration prevents epithelial cell migration and provides connective tissue attachment on the root surface. Hence it improves the clinical attachment gain and reduces the probing depth. (16)
CONCLUSION
Palato-radicular groove may be symptomatic or asymptomatic. Early detection through meticulous examination by the clinician is the pre-requisite in the management of PRG. Successful management and long term prognosis of treating cases of PRG depends on its extent and the associated loss of attachment. Hence, earlier this hidden route is detected; the better is the prognosis of the tooth.
References:
1. Lee K.W, Lee E.C, Poon K.Y. Palatogingival grooves in maxillary incisors. A possible predisposing factor to localized periodontal disease. Br. Dent J 1968; 124: 14-18.
2. Pecora. J.D, Sousa Neto M.D, Santos T.C., Saquay P.L. In vitro study of the incidence of the radicular groove in maxillary incisors. Braz Dent J 1991; 2: 69-73. 3. Glossary of periodontal terms, edn.
3, Chicago: American Academy of Periodontology, 1992: 22
4. Kogan S.L, The prevalence, location and confirmation of palate-radicular grooves in maxillary incisors. J Periodontal 1986; 57: 231-234
5. Albaricci MF, de Toledo, Zuza EP, Gomes DA, Rossetti EP, Prevalence and features of Palato radicular grooves: An in vitro study . J Int Academy of Periodontology; 2008; 10: 2-5.
6. Everett F.G, and Kramer G.M. The Distolingual groove in the maxillary lateral incisor; a periodontal hazard. J Periodontal 1972; 43: 352-361.
7. Friedman S, Goultschin J. The radicular palatal groove. A therapeutic modality. Endod Dent Traumatol 1988; 4: 282-286.
8. Huumonen S, Kvist T, Grondahl K, Molander A Diagnostic value of computed tomography in re-treatment of root fillings in maxillary molars. Int Endo J 2006; 39: 827-833.
9. J. H, Glick D.H, and Frank A.L, Predictable endodontic and periodontal failures as a result of radicular anomalies. Oral Surg.1971; 31: 823-827.
10. Maldonado A, Swartz ML, Phillips RW. An in vitro study of certain properties of a glass ionomer cement. J Am DentAssoc 1978; 96: 785-791.
11. Vermeersch G, Leloup G, Delmee M, Vreven J Antibacterial activity of glassIonomer cements, compomers and resin composites: relationship between acidity and material setting phase. J Oral Rehabil 2005; 32: 368-374.
12. Dragoo MR. Resin Ionomer and Hybrid ionomer cements: Part II. Human clinical and histologic wound healing responses n specific periodontal lesions. International Journal of Periodontics and Restorative Dentistry 1997; 17: 75-87.
13. Elanchezhian S., Harikaran J, Boris Bhim. Platelet rich plasma in the management of palatogingival groove 2011; 1(2): 125-128.
14. Rethman MP. Treatment of palatogingival groove using enamel matrix derivative. Compend Contin Educ Dent. 2001; 22(9): 792.
15. Joseph Choukroun, Antoine Diss, Steve L. Dohan, Anthony J. J. Dohan, Jaafar Mouhyi et al. Platelet-rich Fibrin (PRF): A Second generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg, Oral Med, Oral Pathol, Oral Radiol 2006; 101: E56-60.
16. Anderegg CR, Meltzer DG.: Treatment of the palato-gingival groove with guided tissue regeneration. Report of 10 cases. J Periodontol 1993 ; 64: 72-74.
LIST OF FIGURES
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License