IJCRR - 5(7), April, 2013
Pages: 34-41
Date of Publication: 18-Apr-2013
Print Article
Download XML Download PDF
CERVICAL TRACTION REDUCES PAIN AND DISABILITY IN PATIENTS WITH UNILATERAL CERVICAL RADICULOPATHY
Author: Subhash Chandra Rai, Ajith S., K.R. Bhagavan, Deepak Pinto
Category: Healthcare
Abstract:Background and purpose: Cervical radiculopathy is a common clinical diagnosis classified as a disorder of nerve root and is a pathologic process consisting of pain. A multitude of physical therapy intervention has been proposed to be effective in the management of cervical radiculopathy, including mechanical cervical traction, manipulation, therapeutic exercises and modalities. The aim of the study is to find out the effectiveness of cervical traction along with conventional therapy in the management of cervical radiculopathy. Study Design: Experimental Materials and Methods: Subjects were assigned randomly to one of two groups, each group consisting of 15 subjects. Group I, received TENS and cervical neck exercise. Group II received TENS, cervical neck exercise and intermittent cervical traction. Pre post assessment is done by Neck disability index (NDI) and Visual analogue scale (VAS) Results: The pre test evaluation showed that, there is no significant difference (P> 0.05) between the two groups for all the variables measured. The post-test evaluation of both groups showed a very high significance (P< 0.05) within the group for all the outcome measurements. A post-test comparison of measured variables, between the groups showed that the Group II demonstrated a statistically significant (P< 0.05) reduction in self rated pain and Neck Disability Index. Conclusion: The authors concluded that, even though TENS and neck exercise are effective, the addition of intermittent cervical traction with TENS and exercise is even more effective in the management of cervical radiculopathy and that ICT should have a place in the management of cervical radiculopathy.
Keywords: Cervical radiculopathy, intermittent cervical traction, Conventional therapy
Full Text:
INTRODUCTION
Cervical radiculopathy is a common clinical diagnosis classified as a disorder of nerve root and is a pathologic process which has been defined as pain in the distribution of a specific cervical nerve root caused by nerve root compression from a space occupying lesion such as disc herniation, spondylitic spur, or cervical osteophyte1,2,3 . In a more in depth definition, it encompasses important symptoms other than pain, such as paresthesia, numbness and muscle weakness in dermatomal or myotomal distribution of an affected nerveroot. 4 Cervical radiculopathy is one of the most common health related complaints. 5, 6, 7 . Cervical disk herniation and cervical spondylosis have been described as the main causes of cervical radiculopathy in the literature8,9, and the most frequently involved nerve roots are cervical 6 (C6) and cervical 7 (C7) roots which are typically caused by C5-C6 or C6-C7 disc herniation or spondylosis7,10 . Although patients with cervical radiculopathy may have complaints of neck pain, the most frequent reason for seeking medical assistance is arm pain. 11, 12 . The first choice of management of cervical radiculopathy is non-operative, and various noninvasive interventions have been used with mixed results. The usual treatment of choice is physiotherapy, though in recent years manual therapy is being increasingly used, again with mixed outcomes and probably with an element of risk13. A multitude of physical therapy intervention has been proposed to be effective in the management of cervical radiculopathy, including mechanical cervical traction, manipulation, therapeutic exercises and modalities14, 15 . There are no studies to support or reject the above protocols and also to establish the superiority of one over the other. Further, a combination of TENS, cervical traction and cervical exercise in the management of cervical radiculopathy might give better results than any one of the protocols alone. However there is no comparative study done to find out the effectiveness of conventional therapy versus conventional therapy combined with mechanical intermittent cervical traction on cervical radiculopathy so the aim of our study is to compare the effects between the conventional physiotherapy and intermittent mechanical traction with effects of using conventional Physiotherapy alone on unilateral cervical radiculopathy.
MATERIALS AND METHODS
This study was approved by the Institutional Ethical Committee. 30 subjects from the outpatient department of a teaching hospital, who were diagnosed by the orthopedic surgeon as having unilateral cervical radiculopathy, were selected for the study. The diagnosis was confirmed by assessment with the special tests for unilateral cervical radiculopathy; the subjects were assigned to one of two groups using random sampling method. Both groups consisted of 15 subjects each of both gender .All the patients selected for the study were in the age group 45 to 65 years. We included the subjects with patients diagnosed of having unilateral cervical radiculopathy, unilateral arm pain lasting more than one month, positive foraminal compression test, positive maximal cervical compression test, positive cervical distraction test, and positive Jackson’s compression test. We excluded the subjects with previous cervical fractures or dislocations, cervical tumors, whiplash injuries, spinal cord injury and disorders, bilateral cervical radiculopathy or unilateral radiculopathy lasting less than one month, patients who had undergone spinal surgeries, structural defects of the vertebral column, infective or inflammatory arthritis of the vertebral column, Pott’s spine, osteoporosis, cervical sprain or strain, vertebro-Basilar insufficiency, brachial plexus lesions, thoracic outlet syndrome, spinal deformities, patients with cardiovascular instability and patients with cognitive problems.
Interventions
Group I was treated with Transcutaneous Electrical Nerve Stimulation (TENS) and active neck exercises. TENS was applied with the patient in prone position, we selected pulsed current with rectangular, monophasic shape of pulse, pulse duration was 0.1 msec with pulse frequency of 4pps, and we gradually increased the amplitude until a strong muscle contraction was produced. The duration of treatment was 30 minutes with the frequency of five times/ week for two weeks. Active neck exercise for strengthening was given for the superficial neck flexor, deep neck flexor, lower and middle trapezius, serratus anterior and isometric neck exercises.
Group II was treated with traction, active neck exercises and TENS.the protocol for TENS and active exercise was same as for Group I. Traction was given in supine lying, with a towel roll kept under the neck to maintain the neck in 15 degree flexion. A traction force of 1/10 of the body weight in kg was applied. Traction hold time was set at 40 seconds and rest time at 10 seconds. Duration of traction was 15 minutes/day. The frequency of treatment was 5 days/week for two weeks.
Outcome measurements
All the subjects were evaluated for level of self reported pain and neck disability before the commencement of interventions and at the end of two weeks of interventions. Pain was measured using a 100 mm Visual Analogue Scale(VAS). The subjects were told to mark the intensity of the pain perceived on the scale. Neck disability was measured using the Neck Disability Index (NDI).
Statistical Analysis
The collected data were analyzed using the statistical tests. The data collected by NDI were analyzed using parametric tests as the data was interval in nature. The intra group pre and posttest data for NDI were analyzed using paired ttest, while the post-test inter group data were analyzed with unrelated t-test. The data collected by visual analog scale were analyzed using non-parametric tests as the data is ordinal in nature. The intra group pre and posttest VAS scores was analyzed using Wilcoxon signed rank test, and post-test inter group VAS scores were analyzed with Mann Whitney U-test. The statistical significance or the P value for all the analyzed data was fixed at 0.05.
RESULTS
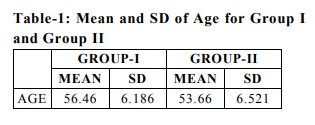
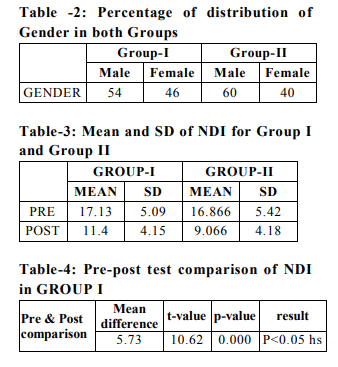
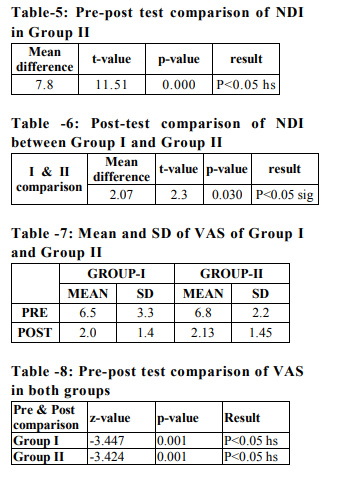
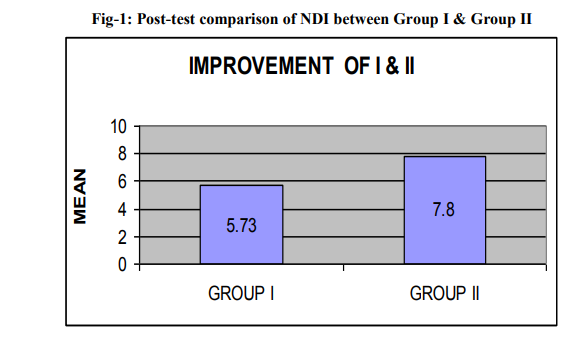
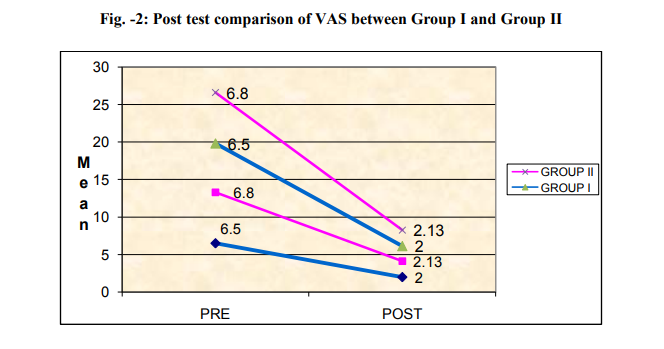
The mean age for Group I was 56.46±6.19 and Group B was 53.66±6.52 as shown in Table1.Group I consisted of 15 subjects (n = 15), with a gender distribution of 8 males (54%) and 7 females (46%). Group II also consisted of 15 subjects (n=15) and a gender distribution of 9 males (60%) and 6 females (40%). These data were presented in Table-2. The mean and the standard deviation (SD) of pre and post-test NDI scores for both, Group I and Group II are presented in Table -3. Compared with the base line, the post-test mean NDI score for Group I was 11.14±4.15 and Group II was 9.06±4.18.The intra group pre and post-test analysis of the NDI score in Group I shows a mean difference of 5.73 (t = 10.62, p= 0.00), which is highly significant statistically (p < 0.05). These results are presented in Table-4.The intra group pre and post-test analysis of the NDI score in Group II shows a mean difference of 7.8 (t = 11.51, p= 0.00), which is highly significant statistically (p < 0.05). These results are presented in Table-5. The results presented in Table -6, and Fig-1 shows the post-test comparison of the NDI scores between Group I and Group II. Group II shows a higher mean difference of 2.07 (t= 2.3, p = 0.03) than Group I which is statistically significant (P>0.05). The mean and the standard deviation (SD) of pre and post-test VAS scores for both, Group I and Group II are presented in Table-7. Compared with the base line, the post-test mean VAS score for Group I was 2.0±1.4 and Group II was 2.13±1.45.The intra group pre-post test comparison of VAS score for group I (z= -3.447, p= 0.001), shows a statistically highly significant reduction (P<0.05) in reported rate of pain after two weeks of interventions. These results are presented in Table-8. The pre-post test comparison of VAS score for Group II (z= -3.424, p= 0.001), shows a statistically highly significant reduction (P < 0.05) in reported rate of pain after two weeks of interventions. The post test comparison of VAS score between the two groups reveals that Group II fared better than group I (u=47, p = 0.005), in the rate of reduction of pain (P<0.05), which is statistically significant as presented in Fig-2.
DISCUSSION
Physical therapy such as heat, ultrasound, TENS, exercise, and cervical collar, either alone or in combination constitute the mainstay of the conservative management of chronic neck pain. There are little established guidelines or protocols available in the literature, as evidenced by one cross sectional study done in Spain finding as many as 35 guidelines and 325 recommendations, with only 20.9% of recommendations considered as evidence based5. Most of the literature concentrates on neck pain in general and very few are available targeting cervical radiculopathy specifically. One of the common protocols used for the management of cervical radiculopathy is a combination of TENS and neck exercise. Cervical traction has also been used increasingly, as the distraction achieved in the cervical vertebrae can probably reduce or remove the impingement on the nerve roots by osteophytic spurs or herniated discs. The results of this study revealed that both groups demonstrated a highly significant improvement in reducing pain as measured by VAS (P<0.05) and decreasing neck disability and improving functional activities as measured by NDI (P<0.05). Further it showed that, the reduction in pain and neck disability is significantly more in the ICT combined with conventional physiotherapy group when compared against the conventional physiotherapy group (P<0.05). Both groups demonstrated a highly significant reduction in both neck and arm pain as measured by VAS (P=0.001) and neck disability as measured by NDI (P = 0.000). The probable reason for the highly significant reduction in the pain could be due to the combination of analgesic effects of TENS and the release of nerve root compression by ICT and the strengthening of neck and scapulothoracic muscles. The analgesic effects of TENS in acute and chronic neck pain and radiating or radicular pain have been well documented by the studies done by Carrol EN et al 16 , Chiu TT et al17 , Slukka KL et al18 , and Nordemer and Thorner19 . The possible mechanism of non-acute pain relief by low rate TENS at motor level stimulation is peripheral block or activation of central inhibition. The induction of rhythmic contraction may also activate the endogenous opiate mechanisms of analgesia. The magnitude of the induced muscle contraction varies from barely perceptible to extremely strong. The effect of mechanical intermittent cervical traction on reducing neck and arm pain and neck disability in cervical radiculopathy is well documented in previous studies done by Joghataei & Arab20, Olivero WC et al21 , Swezey RL et al22 , Browder et al 23 , Cleland JA24 . The possible reason for this conflicting result might be due to variation in the treatment parameters and flaws in the research designs as concluded by Graham et al 25 in a review. The mechanism by which ICT reduces neck and arm pain is possibly by unloading the components of the spine by stretching muscles, ligaments and functional units, reducing adhesions within the dural sleeve, nerve root decompression within the central foramina, and increasing joint mobility. Traction also decreases intervertebral disc pressure as stated by Saunders. Reduced tonic muscle contraction and improved vascular status in the epidural space and perineural structures may also reduce pain. The effect of neck exercises in reducing pain in chronic neck pain and cervical radiculopathy is well documented in the studies carried out by Nikander R et al26 . Further, the study revealed that addition of intermittent cervical traction to TENS and strengthening exercises produces significant decrease in neck and arm pain (P=0.005) and neck disability (P=0.030) when compared to TENS and exercise alone. Though, there are no revious studies to support this result it can be surmised that the possible mechanism by which ICT reduces neck and arm pain such as reducing adhesions within the dural sleeve, and intervertebral disc pressure, nerve root decompression within the central foramina, and increasing joint mobility, when added to the analgesic effects of TENS and the postural stabilization effects of strengthening exercise is better than TENS and strengthening exercise alone in reducing neck and arm pain and neck disability The study duration was short, only 2 weeks, and the results apply to short term only, which might differ in the longer run. Sample size taken for the study is small and bigger sample might have led to some differences in the results. All the measurements were taken manually and this may introduce human error which might affect the reliability.
Scope for further study
We suggest a long term study to make the results more reliable, possibly with regular follow ups over a longer period of time. A large sample size should be taken to improve the consistency of results. More research is necessary with larger groups, standardization of treatment interventions, using more parameters of outcome measurements, matching of subjects, using a control group and blinding to validate the relative merits of the two protocols is also suggested.
CONCLUSION
We conclude that, intermittent cervical traction should have a place in the management of cervical radiculopathy along with TENS and neck exercises in reducing both neck and arm pain and neck disability and in improving activities of daily living.
ACKNOWLEDGEMENTS
Authors would like to thank the Department of Orthopaedics K S Hegde hospital and the participants for their support. Authors acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript. Conflict of Interest: Authors agree that there was no source of conflict of interest.
References:
1. Ellenberg MR, Honet JC, Treanor WJ. Cervical radiculopathy. Arch Phys. Med Rehabil. 1994; 75:342-352.
2. Wainner RS, Gill H: Diagnosis and non operative management of cervical Radiculopathy: J Orthop Sports Phys.Ther. 2000 Dec; 30(12):728-44.
3. Farmer JC, Wisneski RJ. Cervical spine nerve root compression. An analysis of neuroforaminal pressures with varying head and arm positions. Spine. 1994;19:149-158.
4. Garvey TA, Eismont FJ. Diagnosis and treatment of cervical radiculopathy and myelopathy. Orthop-Rev. 1991; 10:595-603.
5. Kondo K, Molgaard CA, Kurland LT, Onofrio BM. Protruded intervertebral cervical disc: incidence and affected cervical level in Rochester, Minnesota, 1950 through 1974. Minn Med. 1981; 64:751-53.
6. Radhakrishnan K, Litchy WJ. O Fallon WM, Kurland LT. Epidemiology of Cervical radiculopathy. A population based study from Rochester, Minnesota, 1976 through 1990. Brain 1994; 117(2): 325-335.
7. Hunt WE, Miller CA. Management of Cervical radiculopathy. Clin Neuro-Jur. 1986; 33:485-502.
8. Yu YI, Woo E, Huang CY, Cervical Spondylotic myelopathy and radiculopathy. Acta Neurol Scand. 1987; 75: 367-73.
9. Abdulwahab S. The effect of reading and traction on patients with cervical radiculopathy based on electrodiagnostic testing. J Neuromusculoskeletal Syst. 1999; 7:91-96.
10. Henderson C, Hennessy R. Posterolateral foraminatomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. 1983; 13:504.
11. Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ. Impact of neck and arm pain on overall health status Spine.2003; 28; 2030-2035.
12. Honet JC, Puri K. Cervical radiculitis: treatment and results in 82 patients. Arch Phys Med Rehabil.1976; 57:12-16.
13. Moffett J, McLean S. The role of physiotherapy in the management of nonspecific back pain and neck pain. Rheumatology. 2006; 45(4): 371-378.
14. Cleland JA, et al: Manual Physical therapy Cervical traction, and strengthening exercise in patients with cervical radiculopathy: a case series: J Orthop Sports Phys. Ther. 2005; 35(12):802-11.
15. Nadler SF. Nonpharmacologic management of pain. JAOA. 2004; 104(11): 6-12.
16. Low J, Reed A. Electrotherapy explained: Principles and Practice. Oxford: ButterworthHeinmann; 2000:113-114.
17. Carrol EN, Badura AS. Focal intense brief transcutaneous electric nerve stimulation for treatment of radicular and postthoracotomy pain. Arch Phys Med Rehabil. 2001; 82:262- 4.
18. Chiu TT, Hui-Chan CW, Chein G. A randomized clinical trail of TENS and exercises for patients with chronic neck pain. Clin Rehabil.2005; 19(8):850-60.
19. Sluka KA, Bailey K, Bogush J, Olson R, Ricketts A. Treatment with either high or low frequency TENS reduces the secondary hyperalgesia observed after injection of kaolin and carrageenan into the knee joint. Pain. 1988; 77(1): 97-102.
20. Nordemer R, Thorner C. Treatment of acute cervical pain – a comparative group study. Pain. 1981; 10(1):93-101
. 21. Joghatataei MT, Arab AM, Khaskar H. The effect of cervical traction combined with conventional therapy on grip strength on patients with cervical radiculopathy. Clin Rehabil. 2004; 18:879-887.
22. Olivera WC, Dulebohn SC. Results of halter cervical traction for the treatment of cervical radiculopathy: retrospective review of 81 patients. Neurosurg Focus. 2002; 12: clinical part 1.
23. Swezey RL, Swezey AM, Warner K. Efficacy of home cervical traction therapy. Am J Phys Med Rehabil. 1999; 78(1): 30-32.
24. Cleland JA, et al: Manual Physical therapy Cervical traction, and strengthening exercise in patients with cervical radiculopathy: a case series: J Orthop Sports Phys Ther. 2005; 35(12):802-11.
25. Graham N, Gross AR, Goldsmith C. Mechanical traction for mechanical neck disorders: A systematic review. J Rehabil Med. 2006; 38(3): 145-152.
26. Nikander R, Malkia E, Parkkari J, Heinonen A, Starck H, Ylinen J. Dose-response relationship of specific training to reduce chronic neck pain and disability. Med Sci Sports Exerc. 2006; 38:2068-2074.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License