IJCRR - 5(11), June, 2013
Pages: 49-55
Date of Publication: 18-Jun-2013
Print Article
Download XML Download PDF
RISK FACTORS ASSOCIATED WITH LOW BIRTH WEIGHT IN NEWBORNS: A TERTIARY CARE HOSPITAL BASED STUDY
Author: Archana Paliwal, Veerbhan Singh, Indu Mohan, Ram Chandra Choudhary, Bhupendra Nath Sharma
Category: Healthcare
Abstract:Objective: To estimate the incidence of low birth weight in new born babies in a tertiary care hospital.To determine the maternal factors which could affect the weight of new born baby. Research Design and Methods: Cross sectional study includes all institutional deliveries comprising mothers and their new born babies. Information regarding mother was obtained by personal interview and ANC record data during six months. Results: 796 mothers were studied, a significant association was found between low birth weight and age of mother at the time of admission, parity, literacy level of mothers, birth spacing, ANC check-up, consumption of iron / folic acid, occupation and type of work of mothers, mother having any medical illness like anemia, pregnancy induced hypertension and any previous or present bad obstetric complications. Conclusions: The finding of the present study clearly reveals that low birth weight can be tackled by providing adequate antenatal care to pregnant women in time. To bring more and more women to hospital for deliveries and provide them adequate ANC, this will prove a long way to reduce birth of low birth weight babies.
Keywords: low birth weight, maternal risk factor, literacy, institutional delivery
Full Text:
INTRODUCTION
“There is no indicator in human biology which tells us so much about the past events and the future trajectory of life, as the weight of infant at birth.” -V. Ramalingaswami [ 1] Birth weight is a reliable index of intrauterine growth and is one of the major factor that determines child survival and his physical and mental developments. [2] The alarmingly high neonatal-perinatal loss in India is attributed to several factors, but the leading cause is low birth weight (LBW) babies which accounts for over one third of all neonates.[3] In underdeveloped and developing countries the problem of low birth weight babies is alarming. WHO estimates that globally about 25 millions low birth weight (LBW) babies are born each year comparising 14% of all live birth, nearly 93% of them are in developing countries, where the incidence varies widely.[4] In India 30- 35% babies are LBW and more than half of these LBW new born are full term babies.[5] Low birth weight is part of the complex interaction of such factors as prenatal growth retardation, prematurity, complications of labour and delivery, congenital malformation and adverse prenatal and postnatal social and psychosocial influences. These factors cannot be separated easily to show separate impacts.[6] Low birth weight is a global community health indicator it is imperative that periodic monitoring be under taken to evaluate the impact of preventive health sevices.[7] Low socioeconomic status, maternal undernutrition, anemia and illness, inadequate prenatal care, obstetric complications and maternal history of premature LBW infants have all been reported to influence the occurrence of LBW. These factors operate to various extents in different environment and cultures.[8] Various maternal factors affect the fetus, directly or indirectly and leads to low birth weight. Many of these factors have been well studied, for example age of the mother, parity, spacing, socioeconomic status, diseases complicating pregnancy like toxemia, antepartum hemorrhage, mode of delivery, hydroamnios, oligohydroamnios, blood group incompatibility, premature rupture of membrane, acute and chronic medical disorders like anemia, hyperemesis, chronic urinary tract infection, tuberculosis, diabetes, illegitimacy,smoking during pregnancy or other drug intoxication or alcohol ingestion. With this background, it was realized to conduct a study on birth weight and associated factors for children born at our institute.
MATERIAL AND METHOD
It is a cross sectional study, which was carried out at M. G. Hospital, Sitapura, Jaipur. This institute provides tertiary health care and specialized medical care to population of South Jaipur zone (semi-urban).Study was conducted in the department of Obs and Gyane at Mahatma Gandhi Medical College and Hospital (MGMC and H), Sitapura, Jaipur during Six Months. Study population was all institutional deliveries comprising mothers and their new born babies. Information regarding mother obtained by personal interview and ANC record data. MGMCandH is a tertiary level institute attached with medical college.
METHOD
Before starting the study, the permission of the hospital ethical committee was taken and informed verbal consent was obtained from all the patients included in the study. All pregnant ladies, attending Mahatma Gandhi Hospital for delivery during study period were examined and interviewed within 24 hours after child birth. Neonates were followed up in hospital, till their stay. In case of discharge from hospital, contact was made telephonically or by home visits whichever was feasible. Pre-structured and pretested protocol was used for collection of information. Regarding mother, information was collected regarding identification, religion, occupation, socio-economic status, literacy status and type of work, type of family, residential environment, life-style and past and present obstetric record, medical history, details of present delivery, complications if any during delivery. Regarding new-born, information regarding birth weight in 1st hour, sex, APGAR scoring, general condition, anthropometric measurements. APGAR score: An APGAR score access how well a newborn is doing at 1 and 5 minutes after birth. The five factors were evaluated.Here are the APGAR factors:
- A = appearance: The skin color should be pinkish.
- P = pulse: The pulse should be 140–160 beats per minute.
- G = grimace: After stimulation, the newborn should pull away or maybe give a good cry.
- A = activity: The arms and legs should be flexed and resist extension.
- R = respiration: There should be a good, loud cry (from the baby, not you).
RESULTS
The alarmingly high neonatal-perinatal loss in India is attributed to several factors, but the leading cause is low birth weight (LBW) babies.
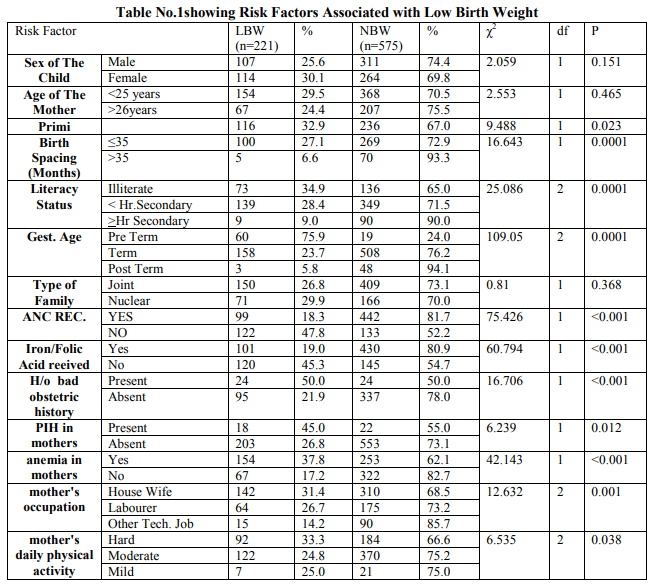
The study was conducted on 796 mothers who delivered in Mahatma Gandhi Hospital, Sitapura, Jaipur within last six months (Jan12 to Jun-12). The information was collected and analyzed, according to our aims and objectives. Out of 796 babies delivered in the hospital 221 (27.72%) were low birth weight and rest 575 (72.24%) were of normal birth weight. In our study the sex ratio was 904/1000. At the time of admission almost 50% mothers belonged to 20-25 years age group with a mean age of 24.75 years. 26.26% mothers were illiterate while 27.51% mothers were educated up to primary and less than 7.29% mothers were graduate and above. 56.78% mothers were house wives, remaining were engaged in agriculture, manual labour, semi professional jobs of other gainful employment. 70.23% mothers were from joint family.66.71% mothers had a family size of 4-9 members. Average number of members in the families of mother was 5.82. 48.12% mothers got married before the age of 18 years with a mean age of marriage 17.8 years. 44.72% mothers had their first delivery up to age of 21 years mean age at time of first delivery 19.60 years. In our study 44.22% of the mothers were primi para 36.06% were second para.Only 17.08% multipara mothers had birth spacing of ≥ 36 months. 51.13% of mothers are anemic according to WHO criteria. 5.03% mothers had the history pregnancy induced hypertension and 24.75% mothers had one of the obstetric complication during their pregnancy. 61.81% mothers performed moderate physical activity during their pregnancy period. Occurrence of low birth weight is slightly higher in female babies (30.16%) than in male babies (25.60%).Occurrence of low birth weight babies was higher in younger age group mothers comparatively. As the mother’s literacy level improved proportion of normal birth weight babies increased. The proportion of low birth weight babies was highest in primi mothers and it is decreased as the parity increased. A significantly higher proportion of normal birth weight babies 81.70% was observed among those who received proper ANC compared to ones who did not, and this association was found statistically highly significant. A significantly higher proportion of normal birth weight babies (80.98%) was observed among those who took iron folic acid during their pregnancy period compared with ones who did not taken and this association was also fount statistically significant. In our present study 480 mothers were second gravida and more. Among them 48 (10%) had previous bad obstetric history. There was significant relation between previous obstetric history and low birth weight babies. It was observed that there was high incidence of obstetric complications in the mothers during present pregnancy who gave birth to LBW babies. Main problem encountered anemia (37.84%), PIH (45%), pre term labour (75.95%).
DISCUSSION
In the present study 796 deliveries and the new born who were delivered in Mahatma Gandhi Hospital, Sitapura, Jaipur within last six months (Jan-2012 to Jun-2012) were taken with the aim and objective of to identify the magnitude of low birth weight babies and to determine the association of maternal and socio-economical factors on the birth weight of babies. In the present study incidence of low birth weight (<2.5kg in first hour of birth) babies was 27.76% similar finding were reported by Kumar M, Paul VK and Deorari A (2002) in a study conducted at sub-district hospital at Ballbhgarh,[9] UNICEF (2006) reported 30% rate in India[10], JS Deshmukh et al (1998) in their study found the prevalence of LBW as 30.3%; Kaushik SL, Parmar VR and Grover N reported 27.8% in 1998.[11,12] Among these low birth weight babies, in our study maximum 20.10% were in the weight group of 2000 to 2499 grams. Proportion of LBW was 25.60% in male and 30.16% in females. In our study there are ratio of female to male was 904/1000. However this difference was not found to be statistically significant. The national sex ratio in 2011 was 940/1000. In our study, mean age of mother at time of admission was 23.82 years (Maximum-37.69% fall in the age group 21-25 years), 28.02% between 26-30 years, 12.19% mothers below 20 years, similar observation had been shown by Uttekar BP et al (2007)[13], Gogoi G and Ahmed FU (2007)[14]. In our study proportion of low birth weight was slightly higher in the age group <20 years but the difference is not statistically significant. Similarly Abner (1982)[15] et al and Fernando and Paul (1987)[16] found no significant association between LBW and maternal age. In present study, 44.22% mothers were primi para, 36.06% mothers were second para and only 1.63% mothers were ≥ fifth para. 1.70% of primi para were <18years. Gogoi G and Ahmed FU (2007) observed a high proportion (12.5%) of primi para belonging to age group of <18 years. [14] The present study showed a high incidence of LBW birth in primi mothers. 116 (52.49%) LBW were born to primi mothers. There is a significant association between parity and low birth weight. Our findings are in accordance with many other workers who also showed this significant association namely Deshmukh JS et al (1998)[11] , Anand K and Garg BS (2006)[17] showed 50% of LBW were born to primi mothers. In our study 26.26% mother were illiterate, 27.51% mothers were educated up to primary, 18.34% up to middle, 15.45% educated up to secondary level and <13% were educated up to higher secondary and above. Uttekar BP et al (2007) also observed in their study in Rajasthan that majority of JSY beneficiaries were illetrate (68%).[13] The present study shows significant association between literacy level of mother and birth weight of their neonate. As the literacy level of mother increased incidence of low birth weight babies decreased and the difference is statistically highly significant. Similar findings are reported by Barker DJP (1998)[18], Joshi SM, Pai NP (2000)[19] . In present study 70.23% mother were from joint family and 29.77% mother were form nuclear families, maximum of number of our study population (46.36%) belong to families having 4- 6 members. Singh A and Arora AK (2007) also found that majority (75.2%) were from joint families in their study in rural North India.[20] In present study there were 48.12% mothers who got married before 18 years age and 37.81% mothers got married at 18-21 years age group. Mean age at marriage in present study was found 17.8 years. However Singh A and Arora AK (2007) observed that 31.6% women had age at marriage <18 years.[20] In our study mean age of first delivery was found to be 19.60 years, NFHS-III (2005-06) reported the same 19.6 years of mean age of first delivery also Singh A and Arora AK (2007) observed 33.4% cases had age at time of first delivery <20 years.[20,21] Our study suggests that as birth spacing between two deliveries increases proportion of low birth weight babies decreases and association was statistically significant. Our findings are in accordance with Mavlankar DV, Gray RH and Trivedi CR (1992) [22] . In present study, there was significant association between occupation and physical activity of mother and proportion of low birth weight babies. Proportion of LBW being higher in mothers engaged in heavy physical activity, Similar observations were found by Launer LJ et al (1990) who highlighted that in developing countries like India, women are responsible for a wide range of house hold work and child care duties as well as work outside the home. These women are also the women at high risk for poor birth outcome. [23] 67.96% mothers in our study had received adequate ante natal care while 32.04% mothers did not receive/inadequate ante natal care. Proportion of low birth weight babies were greater in the mothers who received inadequate ante natal care and association between availing proper ANC checkup and birth weight was found to be statistically highly significant. Joshi HS et al (2005) reported in their study that utilization of ANC (>3 Ante Natal Visit) in 58.20% mothers. There was significant association between birth weight and utilization of ante natal care by mothers. [7] In our present study 66.71% mothers had taken iron and folic acid during their pregnancy.In present study 407 (51.13%) mothers had anemia. Anemia in mothers is indicative of poor socioeconomic status, lack of ante natal care and less spacing, all these factors affect fetal growth and outcome. Most of studies found lower prevalence of anemia like Anand K and Garg BS (2006) reported that 35% of mothers had anemia. [17] Out of 407 anemic mothers, number of low birth babies were 154 (37.84%) which is quite high as compared with non anemic mothers (17.22%). The difference was statistically highly significant. Our finding was also in accordance with Joshi HS et al (2005)[7] . Hypertensive disorder (Gestational Hypertension, Pre-eclampsia and eclampsia) during pregnancy is one of the common causes of chronic placental insufficiency leading to chronic fetal hypoxia and intra uterine growth retardation. In present study 40 (5.03%) mothers were having pregnancy induced hypertension. Out of them number of low birth weight was 18 (45%) which is higher than the mother those were not had pregnancy induced hypertension (26.85%). Finding of our study is in accordance with Samanta Kallol (2006). [24] In the present study a high incidence of bad obstetric history record was observed in mothers delivering low birth weight babies. After excluding primi gravida, it was observed that 151 (33.46%) had previous abortion and 50 (33.11%) of them delivered low birth weight babies. The same was observed other studies; authors Rafati S et al (2005)[8] In the present study 79 (9.92%) babies were born before term (37 weeks) due to spontaneous onset of labour, without any obvious cause, 60 (75.95%) babies out of them were of low birth weight. Other worker have also observed spontaneous onset of labour without obvious cause leading to LBW births. Fernano and Paul (1987) observed such preterm labour in 29.9% cases. [16] 24.75% mothers faced one or the other obstetric complication. Out of them 18.78% had PIH/APH/eclampsia and 16.24% had breech or any other malpresentation, other complications were non-prograssion of labour (5.08%), overdue gestational period (25.38%) , cephalo-pelvic disproportion, fetal distress and oligohydramnios (11.17%). Joshi HS et al (2005) observed lesser frequency of complications among mothers.[7]
CONCLUSION
Of 796 mothers studied, a significant association was found between low birth weight and age of mother at the time of admission, parity, literacy level of mothers, birth spacing, ANC check-up, consumption of iron/folic acid, occupation and type of work of mothers, mother having any medical illness like anemia, pregnancy induced hypertension and any previous or present bad obstetric complications. Bases on the findings of this study following suggestions are made:-The proportion of low birth weight found to be high 27.76%, it can be tackled by providing adequate antenatal care to pregnant women in time. To bring more and more women under Janani Shishu Suraksha Yojna (JSSY) and provide them adequate ANC, this will provide a long way to reduce birth of low birth weight babies.
ACKNOWLEDGEMENT
Authors acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.
References:
1. V. Ramalingaswami; Meharban Singh, “The challenges of low birth weight babies” Care of the new born 6th edition, Sagar Publications, New Delhi 2004 P 219
2. Ramankutty P. Tikreeti RA, Rasaa study on birth weight of Iraqi (Paediatr 1983;29:5-10.
3. Guha’s Neonatology principles and practice IIIrd edition, Jaypee brothers medical publishers (P) Ltd. 2005, P-27
4. Park K’s text book of preventive and social medicine. 21st Edition, Banarasidas Bhanot publishers, Jabalpur 2011, P 494
5. WHO Bridging the gaps, The World Health Report, 1995, Report of the Director General.
6. Overpeck MD, Moss AJ, Hoffman HJ, Hendershot GE. A comparison of the childhood health status of normal birth weight and low birth weight infants. Pub] Hlth Rep 1989;104:58-70
7. H.S. Joshi, Sh Subba, SB Dabral, S Dwivedi, D. Kumar and S Singh ; Risk Factors Associated with Low Birth Weight in Newborns; Indian Journal of Community Medicine Vol. 30, No. 4, OctoberDecember, 2005; 142-143
8. Shiva Rafati MD Hajieh Borman MD Mohammad-Bagher Akhavirad MD, Nader Fallah MSc- 2005
9. Kumar M. Paul, V. K. Deorari A et al Neonatal outcomes at a sub-district hospital in North India. Journal of Tropical Pediatric 2002;48(1)43-6
10. World Health Statistics Quarterly 1984 and State of World Children UNICEF 2006
11. J.S. Deshmukh, D. D. Motghare, S. P. Zodpay and S. K. Wadhva Low Birth Weight and Associated Maternal Factors in urban area, Indian journal of Pediatrics Jan1998 vol-35; 33-35
12. Kaushik Sl, Parmar VR, Grover N et alNeonatal mortality rate; relationship to birth weight and gestational age. Ind J Ped. 1998; 65(3);429-33
13. Uttekar BP, Barge S, Khan W, Deshpande Y, Uttekar V, Sharma J et al. Assessment of ASHA and JSY in Rajasthan. 2007, Apr
14. Gogoi G, Ahmed FU. Effect of Maternal Nutritional Status on the Birth Weight Among Women of Tea Tribe in Dibrugarh District. Indian Journal of Community Medicine, 2007 Apr;32(2):120-122.
15. Abner H, Levkeff, Milton Westphal M, Clinton Miller III Yvome Michal. Maternal risk factors in infants with very low birth weight. Obstet Gynecol 60:612, 91982)
16. Fernando Arias, Paul Tomich. Etiology and outcome of low birth weight and preterm infants. Obstet gynecol 60: 277, 1982
17. Kiran A, Garg B S. A study of factors affecting LBW. Indian Journal of community Medicine 2006
18. Barker DJP. Mothers, babies and health in later life. Edinburgh: Churchill Livingstone; 1998.
19. Joshi SM and Pai NP. Effect of maternal bio-social determinants on the birth weight in a slum area in Mumbai. Ind J. of Com Med. 2000 Jul-Sep;25(3):121-124
20. Singh A, Arora AK. The Changing Profile of Pregnant Women and Quality of Antenatal Care in Rural North India. Indian Journal of Community Medicine, 2007 Apr;32(2):136.
21. NFHS-III (National Family Health SurveyIII), International Institute for Population Sciences, Mumbai, India, 2005-06, pg.191- 222.
22. Mavalankar DV, Gray RH, Trivedi CR. Risk Factors for Preterm and Term Low Birth Weight in Ahmadabad, India. International Journal of Epidemiology, Apr. 1992; 21:263-272
23. Launer LJ, Villar J, Kestler E, de O nis M. The effect of maternal work on fetal growth and duration of pregnancy: a prospective study. British Journal of Obstetrics and Gynaecology 1990; 97 : 62-70.
24. Samanta, Kallol. Study of maternal and parinatal morbidity and mortality in hypertensive disorders complicating pregnancy. Journal of Obstetrics and Gynecology, 2006 Sep. Rajiv Gandhi University of Health Sciences
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License