IJCRR - 5(12), June, 2013
Pages: 61-71
Date of Publication: 28-Jun-2013
Print Article
Download XML Download PDF
COMPARISON OF POSTERIOR SUB-TENON TRIAMCINOLONE WITH INTRAVITREAL BEVACIZUMAB FOR MACULAR EDEMA IN NON-ISCHEMIC RETINAL VEIN OCCLUSIONS
Author: Murali Mohan Gurram
Category: Healthcare
Abstract:Purpose: to compare the efficacy of posterior sub-tenon triamcinolone (PSTT) with intravitreal bevacizumab, when used as the primary treatment for macular edema associated with retinal vein occlusions. The efficacy is studied in improvement of visual acuity and reduction in macular edema. Background: Macular edema is the commonest cause of visual loss in retinal vein occlusions. Many treatments have been advocated including LASER, PSTT etc. with the recent trend being the usage of intravitreal anti VEGF agents and steroids. Methods: In a retrospective comparative case series, the records of patients who received PSTT (group I) and those who received Intravitreal bevacizumab (Group II) for macular edema associated with retinal vein occlusions, between march 2010 and September 2012 were analyzed. Group I had 24 eyes of 24 patients (13 male and 11 female) and group II had 26 eyes of 26 patients (13 male and 13 female). Group I had received Posterior Sub-Tenon injection of Preservative free Triamcinolone Acetonide (40 mg/1 ml) and group II had received intravitreal injection of 1.25 mg/0.05 ml avastin. Changes after four weeks of treatment, in best corrected visual acuity (letters of ETDRS chart) and central macular thickness (time domain OCT measurements) were studied. IOP was also focused on. Results: In group I the BCVA increased from 30.08\?10.16 letters to 40.21 \?8.93 letters with an increase of 10.13 \?8.20 letters (P=< 0.001). The Mean CMT in group I changed from 575.08 \? 131.55 \? to 305.54 \? 157.10 \? with a decrease of 269.54 \? 149.78 \? (P=< 0.001). In group II BCVA increased from 33.81 \? 7.60 letters to 54.89 \? 8.96 letters by 21.08 \? 11.98 letters (P=0.001) and mean CMT decreased from 570.35 \? 115.01 \? to 206.58 \? 22.18 with a change of 363.77 \? 104.71 \? (P=0.004). Group II had better effect both on BCVA and CMT which was statistically significant (P value for BCVA < 0.001 and for CMT 0.013). No major complications were noted in either group. Conclusions: Both PSTT and IVB are effective in decreasing the CMT and increasing the BCVA in cases of macular edema due to Non-ischemic Retinal vein occlusions. IVB is better option, when compared to PSTT as shown by significant P value. But in view of the extraocular nature and less complications reported with PSTT, it can be tried as first line of treatment before contemplating IVB. Multicenter randomized trials with longer follow-up are needed to evaluate the long term safety and efficacy of these treatments.
Keywords: avastin, bevacizumab, intravitreal injection, posterior subtenon injection, Retinal vein occlusion, triamcinolone Acetonide
Full Text:
INTRODUCTION
Retinal vein occlusion (RVO) is second most common retinal vascular disease, only next to diabetic retinopathy.1 In an Indian study, RVOs were detected in 0.8% of adults, with branch retinal vein occlusions (BRVO) being approximately seven times more common than central retinal vein occlusions (CRVO).2 The pathologic site in case of CRVO is behind lamina cribrosa and in BRVO the arteriovenous crossing. Non-ischemic and ischemic are two variants.3The causes for visual loss are macular edema (ME) and ischemia, with Macular edema being the most common cause for visual loss.4 Venous occlusion leads to poor venous drainage, dilatation and tortuosity of the large retinal veins, and increased retinal capillary pressure. These changes lead to secondary inflammation and result ultimately in breakdown of blood retinal barrier with, exudation of blood, fluid, and lipid into the retina, leading to the development of macular edema.5 Role of Vascular Endothelial Growth Factor (VEGF) has been established. The increased backpressure leads to stagnation of blood flow, which leads to hypoxia of retina. This causes release of various chemical agents, of which VEGF is important.6 VEGF is the major vasopermeability factor that disrupts the blood–retina barrier in Retinal vein occlusion (RVO) by inducing fenestrations in capillaries and venules.7 Treatment of ME is very important to improve the vision of the patient. In a study, no case of macular edema with central retinal vein occlusion resolved spontaneously by 1 year, but approximately 30% resolved spontaneously over a long interval, often with neuroretinal or pigment epithelial scarring and atrophy.8 when resolution of ME does occur, it can be long delayed. In one study, the time to resolution of ME in untreated non-ischemic CRVO with ME averaged 23 months compared to 29 months for ischemic CRVO.9 spontaneous resolution of BRVO associated ME is better, but still can lead to macular damage without intervention. 10 Macular grid laser was considered the gold standard treatment. The photocoagulation of the photoreceptors reduces the oxygen consumption of the outer retina and allows oxygen to diffuse from the choroid to the inner retina, where it relieves hypoxia.11 But Central Vein Occlusion Study (CVOS) proved that the macular grid laser is not useful in improving the vision. There was no statistically significant difference between treatment and control visual acuity at any stage of follow-up.12 Branch Vein Occlusion Study (BVOS) Group has advised grid laser for macular edema of more than three months, associated with BRVO. 1 But postponing treatment for more than three months would adversely affect the collaterals, and cause more damage to macula. Therefore early treatment with intravitreal or periocular injections was advised. 13,14 Triamcinolone acetonide is a corticosteroid that, in addition to its anti-inflammatory effects, may cause down-regulation of vascular endothelial growth factor (VEGF).15 Triamcinolone intravitreally was largely used with good results in ME of RVO.16,17 Intravitreal Triamcinolone may be associated with various complications like glaucoma, cataract, endophthalmitis, retinal detachment, scleritis etc.18,19 Since the first report of the efficacy of intravitreal bevacizumab (IVB) in a patient with ME secondary to CRVO in 2005,20 several case series have shown the benefit of this treatment, with an improvement in visual acuity and a decrease of Central Macular Thickness (CMT) in patients with ME with RVO.21 In CRVO, adding triamcinolone to bevacizumab did not have additional benefit when compared to intravitreal bevacizumab alone.22 Need for the operation theatre setup and the cost of anti-VEGF drug may be limiting factors to many patients. As it is an intraocular procedure, it may be associated with severe complications including endophthalmitis, retinal detachment etc. 23,24 Intra-ocular anti-VEGF can be associated even with systemic complications. 25 Posterior subtenon space is adjacent to macular area. The steroid deposited in that area would transfuse through sclera and act on the macular edema. Posterior sub-tenon Triamcinolone has been used for macular edema with good effects. 26, 27 PSTT is a simple outpatient procedure without involvement of huge costs. Most of these patients being poor and unaffordable to costly anti-VEGF injections, can PSTT be tried as an alternative to IVB? This study is aimed to compare the anatomical and visual effects PSTT with intravitreal bevacizumab in macular edema associated with retinal vein occlusions. To the best of our knowledge, this is the first study to compare these two treatment modalities in cases of macular edema associated with non-ischemic vein occlusions.
MATERIALS AND METHODS
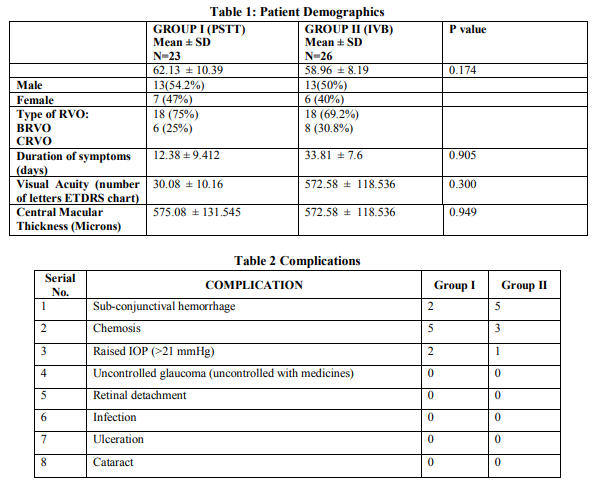
This is a Retrospective comparative interventional case series. Setting is a tertiary eye care in Hyderabad, south India. Duration of study was from March 2010 to September 2012. All the records of macular edema associated with retinal vein occlusions, which received PSTT or IVB as first line of treatment, were analyzed. Macular edema with Non-Ischemic RVO as evidenced by clinical and angiographic evaluation, Decreased vision with vision better than PL and CMT ≥ 250 µ were the criteria to include the records in the study. Ischemic RVO, Prior laser treatment, Glaucoma/Ocular Hypertension, Cataract which precludes the evaluation of macula, Vitreous hemorrhage, Macular ischemia, Iris neovascularization, and Prior intravitreal injections formed the exclusion criteria. Total of 50 records were analyzed. Out of these 50, 24 eyes had received PSTT and the other 26 eyes had received IVB. All these patients had undergone basic pre-procedure eye examination including Best corrected visual acuity with 4 meter ETDRS chart (4m ETDRS chart model no. 2121, Akriti Logistics) with 70 letters in 14 lines, thorough slit lamp examination, Goldman Applanation Tonometry, Contact lens biomicroscopy, Indirect ophthalmoscopy, FFA, and OCT (Time domain OCT, Zeiss Stratus OCT). Demographics of the patients are given in table 1.
TECHNIQUE OF PROCEDURE
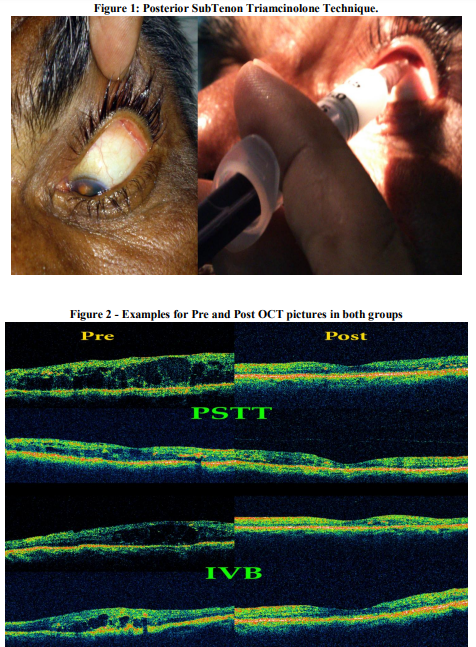
All procedures were done by a single surgeon, the author. The technique used for Intravitreal bevacizumab: All injections were given in sterile environment of operation theatre. Povidone iodine drops were instilled in the eye prior to painting and draping. After placement of eye speculum, measurement is taken which are 3.5mm for pseudophakics and aphakics and 4 mm for phakic eyes. Inferotemporal quadrant is selected. Conjunctiva is displaced and injection is given in a tunneled incision technique.28 1.25 mg of Avastin in 0.05 ml is used from a multidose vial. (Avastin; Genentech Inc., California, USA). The technique of PSTT was as described by Nozik.29 All injections were given as out-patient procedures. Patient is made to lie down comfortably on the treatment couch. Topical anesthesia drops (Proparacaine 0.5%) were instilled twice with 5 minutes interval. First drop is placed in inferior cul-de-sac and the second drop is placed over the superotemporal quadrant, after asking the patient to look inferonasally. 2 ml syringe is loaded with 1ml (40mg) of preservative free Triamcinolone Acetonide (Aurocort, Aurolabs, India). Needle is replaced with a 26G half inch needle. Surgeon positions himself on the opposite side of the patient. Patient is asked to stare at his/her opposite shoulder (Inferonasal gaze). With left hand, surgeon retracts the upper lid upwards, thus exposing the superotemporal quadrant. Needle was passed through the bulbar conjunctiva and tenon’s capsule, at the posterior most visible area, with bevel facing towards globe. Maintaining the needle as close to the globe as possible, needle is advanced. Side to side movement of the needle is made and limbus is looked for any movement. Any movement of the limbus indicates the presence of needle in sclera. Needle is advanced till the hub is reached over the injection site. Aspiration was done to rule out any blood vessel entry, and then the drug is injected with moderate force. See figure 1. Post procedure instructions for all patients were same with oral acetazolamide and NSAID. Topical medications include Steroid-Antibiotic combination for five days and anti-glaucoma medications, usually timolol 0.5% for one month. Acetazolamide 250 mg is given thrice daily for one day. NSAID is given for 2 days. Data from records was collected so that the results after one month of procedure could be analyzed.
OBSERVATIONS
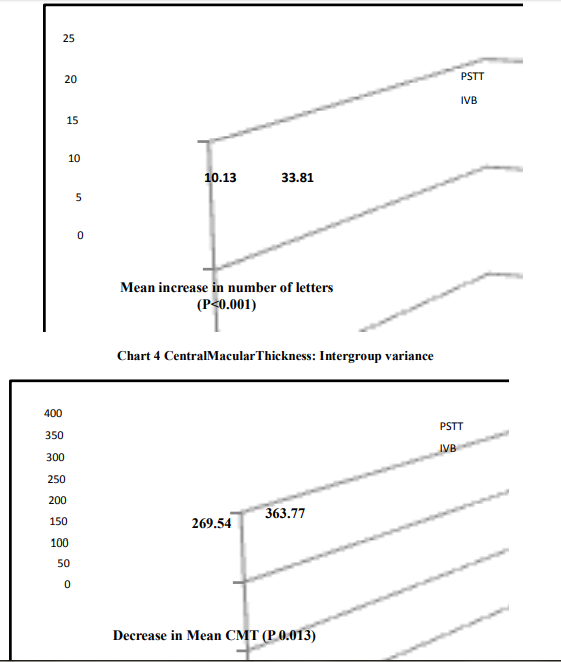
On 1st post op day, 5 patients in group 1 showed chemosis, 2 showed sub-conjunctival hemorrhages and the rest showed no problems. In group II 5 patients had subconjunctival hemorrhage and 3 had chemosis. None of the patients had severe problems like, endophthalmitis, vitreous hemorrhage or retinal lesions. More than 5 letters improvement in BCVA was noted in 16 eyes (66.7%) in group I and 23 (88.46%) eyes in group II. All of them showed at least some amount of reduction in CMT. None of them had any major complications. The pre-op and post-op measurements are charted below: In group I the pre-op Visual acuity was 30.08±10.16 letters (Mean ± Standard deviation) which improved to 40.21 ±8.93 letters. There was increase in the BCVA by 10.13 ±8.20. Visual acuity in group II increased from 33.81 ± 7.60 to 54.89 ± 8.96 letters by 21.08 ± 11.98. The Central Macular thickness in group I changed from 575.08 ± 131.55 µ to 305.54 ± 157.10 µ with a decrease of 269.54 ± 149.78. Central macular thickness in group II decreased from pro op value of 570.35 ± 115.01 to post op value of 206.58 ± 22.18. The change was 363.77 ± 104.71. Two eyes in group I and one eye in group II had raised IOP which was controlled with additional anti-glaucoma medications. None of the eyes in either group developed any other complications like endophthalmitis, retinal detachment etc. The details of complications are listed in table 2.
STATISTICAL ANALYSIS and RESULTS
Statistical Analysis was made with SPSS software (SPSS for Windows, version 13.0, SPSS Inc., Chicago, Illinois, USA). For the effect on BCVA and CMT in each group, Paired sample statistics was done with 95% confidence interval. Group I BCVA: the mean Pre-Op visual acuity in terms of numbers was 30.08. The standard deviation was 10.164 with standard error of mean 2.075. The Post-Op mean was 40.21 with standard deviation 8.925 and standard error mean 1.822. The pre and Post op were analyzed with paired samples test. The mean change in VA was 10.125 with standard deviation 8.20 and standard error mean 1.674. The 2-tailed significance (P value) was <0.0001 suggesting that PSTT improves the visual acuity which is statistically significant. Group I CMT: The mean Pre-Op central macular thickness was 575.08 microns with standard deviation 131.545 and standard error mean 26.852. The mean post-Op mean was 305.54 microns with standard deviation 157.103 with standard error mean 32.069. The change in central macular thickness was 269.542 microns with standard deviation of 149.779 and P value <0.0001 which suggests that PSTT reduces the central macular thickness to a statistically significant level.
Group II BCVA: The mean Pre-Op BCVA was 33.81 with standard deviation of 7.60 and standard error mean of 1.49. The Mena Post-Op BCVA was 54.88 with standard deviation of 8.959 and standard error mean of 1.757. The change in BCVA was 21.077 with standard deviation of 11.976 and standard error mean of 2.349. The P value was <0.001 which is highly significant. This suggests that intravitreal avastin brings an increase in visual acuity by one month. Group II CMT: the mean Pre-Op CMT was 570.35 with standard deviation 115.01 and standard error mean 22.55. Post op mean was 206.58 with standard deviation 22.18 and standard error mean 4.35. The paired samples test analysis shows a mean change of 363.769 microns with standard deviation of 104.715. P value was <0.001 which is highly significant, suggesting that IVB therapy brings down the macular thickness significantly. Intergroup analysis was done using “Independent samples test” with Levene’s test for equality of variances. With regards to BCVA the mean increase in BCVA in group I was 10.13 and in group II was 21.08. Group II had better effect which was statistically significant with the P value being <0.001. With regards to CMT the mean decrease in group I was 269.54 and in group II was 363.77. Group II again had more effect in decreasing the CMT with significant P value 0.013.
DISCUSSION
Macular edema is the most common cause for decreased vision in patients with RVO. The macular edema is of vasogenic edema unlike in ischemic RVO where the edema is cytotoxic macular edema. Due to vein obstruction, blood stagnates in the venous system, thus increasing the pressure in capillary system leading to derangement in starling’s forces. These changes also lead to secondary inflammation and result ultimately in breakdown of blood retinal barrier with, exudation of blood, fluid, and lipid into the retina, leading to the development of macular edema. Many cytokines are involved in this process which includes VEGF, TGF, TNF, PDGF, IL-6, FGF etc. VEGF is the major vasopermeability factor that disrupts the blood–retina barrier in RVO by inducing fenestrations in capillaries and venules. Average vitreal concentration of VEGF in CRVO is 8.6 ng/ml in CRVO, 2.0 ng/ml in BRVO compared to 0.26 ng/ml in normal eyes.30 A lower concentration of intraocular VEGF is required to increase vascular permeability than that required to induce neovascularization. Untreated macular edema in RVO typically persists for a long time. In one study, the median time to macular edema resolution was 23 months for nonischemic CRVO and 29 months for ischemic CRVO.9 Chronic macular edema and macular cysts in CRVO can result in a lamellar or full thickness macular hole.31 Early treatment of macular edema may be better for visual improvement before longstanding macular edema results in irreversible photoreceptor damage 32 Intravitreal Triamcinolone and anti-VEGF agents are being used since past many years.20,32 Posterior sub-tenon Triamcinolone has been used for many indications like DME, Uveitis etc. 26,27 In a prospective study, Nil etal. evaluated the efficacy of PSTT 24 eyes with macular edema secondary to RVO. They concluded that PSTT was an effective therapeutic method to treat ME associated with RVO.33 Lin etal. , in a prospective, non-comparative study have treated 18 eyes of 18 patients of severe CME with recent onset CRVO, with PSTT. They concluded that PSTT is effective in reversing CME and improving VA in recent-onset CRVO. They also recommended early treatment before longstanding macular edema results in irreversible photoreceptor damage. 34
To the best of our knowledge, this comparative study is the first of its kind, where PSTT is compared with IVB.
CONCLUSION
Both PSTT and IVB are effective in decreasing the CMT and increasing the BCVA in cases of macular edema due to Non-ischemic Retinal vein occlusions. IVB is better, when compared to PSTT. But in view of the extraocular nature and less complications reported with PSTT, the high cost of IVB, the complications associated with IVB, PSTT can be tried as first line of treatment before contemplating IVB. Multicenter randomized trials with longer follow-up are needed to evaluate and compare the long term safety and efficacy of these treatments.
ACKNOWLEDGMENTS
Author is thankful to Mr. Venkat Ram, ophthalmic assistant for his help in various ways, in patient care. Author acknowledges the great help received from the scholars whose articles cited and included in references of this manuscript. The author is also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Author is grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.
References:
1. The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984;98:271-282.
2. Jonas JB, Nangia V, Khare A, Sinha A, Lambat S. Prevalence and associations of retinal vein occlusions: the Central India Eye and Medical Study. Retina 2013; 33(1):152-9.
3. Sohan Singh Hayreh. Retinal vein occlusion. IJO 1994;42(3):109-32.
4. The Central Vein Occlusion Study Group. Natural history and clinical management of central retinal vein occlusion. Arch Ophthalmol. 1997;115:486-491.
5. Lee HB, Pulido JS, McCannel CA, Buettner H. Role of inflammation in retinal vein occlusion. Can J Ophthalmol. 2007;42(1):131-133.
6. Behzadian MA, Wang XL, Al-Shabrawey M, Caldwell RB. Effects of hypoxia on glial cell expression of angiogenesis-regulating factors VEGF and TGF-beta. Glia. 1998;24:216–25
7. Schlingemann RO, van Hinsbergh VWM. Role of vascular permeability factor/vascular endothelial growth factor in eye disease. Br J Ophthalmol. 1997;81:501– 12
8. McIntosh RL, Rogers SL, Lim L, Cheung N, Wang JJ, Mitchell P, Kowalski JW, Nguyen HP, Wong TY. Natural history of central retinal vein occlusion: Evidence -based systematic review. Ophthalmology. 2010;117:1113–23
9. Hayreh SS, Podhajsky PA, Zimmerman MB. Natural history of visual outcome in central retinal vein occlusion. Ophthalmology. 2011; 118:119–33.
10. Haller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jacques ML, Jiao J, Li XY, Whitcup SM: OZURDEX GENEVA Study Group: randomized, shamcontrolled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology 2010; 117: 1134–1146.
11. Arnarsson A, Stefánsson E. Laser treatment and the mechanism of edema reduction in branch retinal vein occlusion. Invest Ophthalmol Vis Sci. 2000; 41:877–9.
12. The Central Vein Occlusion Study Group. Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion: The Central Vein Occlusion Study Group M report. Ophthalmology. 1995; 102: 1425-33.
13. Oh JY, Seo JH, Ahn JK, Heo JW, Chung H. Early versus late intravitreal triamcinolone acetonide for macular edema associated with branch retinal vein occlusion. Korean J Ophthalmol 2007; 21:18-20.
14. Lin JM, Chiu YT, Hung PT, Tsai YY. Early treatment of severe cystoid macular edema in central retinal vein occlusion with posterior sub-tenon triamcinolone acetonide. Retina 2007; 27:180-189.
15. Nauck M, Roth M, Tamm M, et al. Induction of vascular endothelial growth factor by platelet-activating factor and platelet-derived growth factor is down regulated by corticosteroids. Am J Resp Cell Mol Biol. 1997; 16: 398-406.
16. Ip MS; Gottlieb JL; Kahana A; Scott IU; Altaweel MM; Blodi BA; Gangnon RE; Puliafito CA. Intravitreal triamcinolone for the treatment of macular edema associated with central retinal vein occlusion. Arch Ophthalmol. 2004; 122(8):1131-6 (ISSN: 0003-9950)
17. Karacorlu M, Ozdemir H, Karacorlu SA. Resolution of serous macular detachment after intravitreal triamcinolone acetonide treatment of patients with branch retinal vein occlusion. Retina 2005; 25:856-860.
18. Konstantopoulos A, Williams CP, Newsom RS, Luff AJ. Ocular morbidity associated with intravitreal trimcinolone acetonide. Eye (Lond). 2007; 21(3): 317-320.)
19. Ozkiri A, Erkiliç K. Complications of intravitreal injection of triamcinolone acetonide. Can J Ophthalmol 2005; 40:63- 68.
20. Rosenfeld PJ, Fung AE, Puliafito CA. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central vein occlusion. Ophthalmic Surg Lasers Imaging 2005;36:336–9
21. Hsu J, Kaiser RS, Sivalingam A, et al. Intravitreal bevacizumab (avastin) in central vein occlusion. Retina 2007;27:1013–9.
22. Murali Mohan Gurram. Effect on macular edema in non-ischemic CRVO: Comparison Between Intravitreal Bevacizumab And Combined Intravitreal Bevacizumab And Triamcinolone. Journal of Evolution of Medical and Dental Sciences. 2013; 2(18): 3293-3304.
23. Meyer CH, Michels S,Rodrigues EB, Hager A, Mennel S, Schmidt JC etal. Incidence of rhegmatogenous retinal detachments after intravitreal antivascular endothelial factor injections. Acta Ophthalmol. 2011; 89(1):70-5.
24. Artunay O; Yuzbasioglu E; Rasier R; Sengül A; Bahcecioglu H. Incidence and management of acute endophthalmitis after intravitreal bevacizumab (Avastin) injection. Eye (Lond). 2009; 23(12):2187-93
25. Shima C; Sakaguchi H; Gomi F; Kamei M; Ikuno Y; Oshima Y; Sawa M; Tsujikawa M; Kusaka S; Tano Y. Complications in patients after intravitreal injection of bevacizumab. Acta Ophthalmol. 2008; 86(4):372-6
26. Bakri SJ, Kaiser PK. Posterior subtenon triamcinolone acetonide for refractory diabetic macular edema. Am J Ophthalmol 2005;139:290–294
27. Helm JH, Holland GN. The effects of posterior sub tenon injection of triamcinolone acetonide in patients with intermediate uveitis. Am J Ophthalmol 1995; 120:55-64.
28. Rodrigues EB, Meyer CH, Grumann A Jr, Shiroma H, Aguni JS, Farah ME. Tunneled scleral incision to prevent vitreal reflux after intravitreal injection. Am J Ophthalmol 2007; 143:1035-1037.
29. Nozik RA. Periocular injection of steroids. Trans Am Acad Ophthalmol Otolaryngol 1972; 76:695-705.
30. Ehlken C, Rennel ES, Michels D, et al. Levels of VEGF but not VEGF 165b are increased in the vitreous of patients with retinal vein occlusion. Am J Ophthalmol. 2011; 152:298–303.
31. Shukla D, Rajendran A, Kim R. Macular hole formation and spontaneous closure after vitrectomy for central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2006; 244:1350–2.
32. Lee, henry; shah, gaurav k. Intravitreal Triamcinolone As Primary Treatment of Cystoid Macular Edema Secondary to Branch Retinal Vein Occlusion Retina: July/August 2005 - Volume 25 - Issue 5 - pp 551-555
33. Lin JM, Chiu YT, Hung PT, Tsai YY. Early treatment of severe cystoid macular edema in central retinal vein occlusion with posterior sub-tenon triamcinolone acetonide. Retina. 2007 Feb; 27(2):180-9.
34. Nil ?rem, Mehmet , Cenk, Zeliha, Emin GÜRSEL. Posterior Subtenon Triamcinolone Acetonide in the Treatment of Macular Edema Secondary to the Retinal Vein Occlusion Journal of Retina-Vitreous 2004, Volume 12, Number 3, Page(s) 180- 183


|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License