IJCRR - 5(13), July, 2013
Pages: 80-87
Date of Publication: 17-Jul-2013
Print Article
Download XML Download PDF
COMPLETE OSSIFICATION OF SUPERIOR TRANSVERSE SCAPULAR LIGAMENT: INCIDENCE AND ITS CLINICAL IMPLICATIONS
Author: Parineeta Suman, Raj Kishore Mahato, Sabita Singh, ArunKumar.S.Bilodi
Category: Healthcare
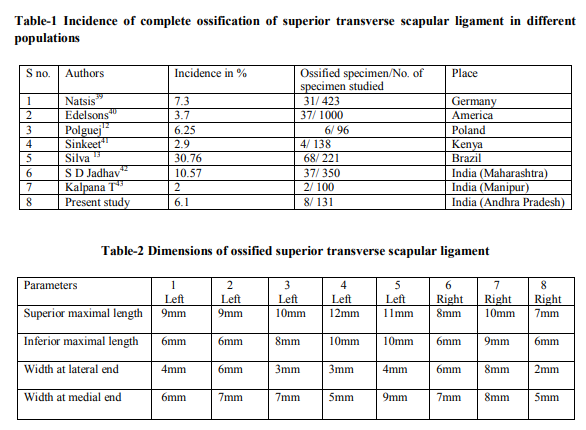
Abstract:Introduction and Aims- The ossified superior transverse scapular ligament is one of the risk factor for the suprascapular nerve entrapment neuropathy and poses a challenge during suprascapular nerve decompression.This study has been done to understand the various mechanisms of neural injury leading to suprascapular entrapment neuropathy and to compare its incidence in different populations. Materials and Methods-131 dryIndianhuman scapulae (64-right and 67-left) were examined and analysed. Results-6.1%(8 in 131) scapulae presented with completely ossified STSLof which 3 on right side and 5 on left side. Conclusion- The anatomical knowledge of ossified STSLmay be helpful for clinician dealing with suprascapularnerve entrapment neuropathy and the knowledge of underlying mechanism of injury to nerve may be helpful in planning the appropriate treatment strategy.
Keywords: Scapula, Superior transverse scapular ligament, Suprascapular notch, Suprascapular neuropathy, ossification.
Full Text:
INTRODUCTION
The superior transverse scapular (suprascapular) ligament is a thin flat fibro-fasciculus band attached laterally to the base of the coracoid process and medially to the medial (inner) side of the suprascapular notch.1,2The ligament and the notch together form a sharp edged inelasticosteofibrous foramen through which suprascapular nerve travels.3,4Suprascapular artery and vein usually pass over the ligament.1,5The classic description of superior transverse scapular ligament (STSL) is a completely non-ossified single band and should be expected on average, in three-fourth of cases.6 The documented variation of STSL includes calcification, partial or complete ossification and multiple bands.6 The ossification of the STSL was considered anomalous by Harris et al.7The size and shape of suprascapular notch may be a factor in suprascapular nerve entrapmentneuropathybecause narrow notch has been found in patient with this neuropathy.8,9 Suprascapular nerve entrapment neuropathy has also been described in clinical scenario without a visible ossification of STSL.10This is characterised by weakness of abduction and external rotation of the arm due to supraspinatus and infraspinatus muscle denervation and frequently accompanied by ill-defined shoulder pain.11 Variable incidence of complete ossification of STSL has been reported by research workers which vary in different population. In Indian scenario paucity ofdata on complete ossification are available. Hence this study has been reported to compare the incidence of ossified STSL in different population, to explain its various mechanismand to discuss its clinical implications.
MATERIALS AND METHODS
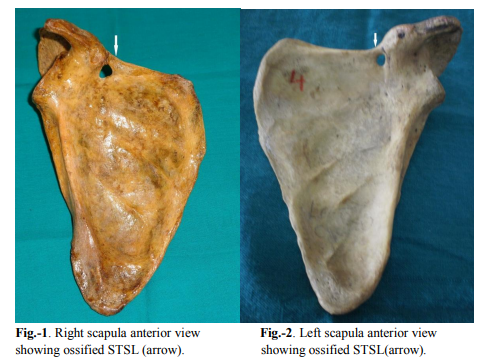
The present study was carried out on 131(Right64, Left-67) dried human scapulae of unknown sex obtained from Department of Anatomy, SVS Medical College,Mahabubnagar, Andhra Pradesh and Raichur Institute of Medical Sciences, Raichur, Karnataka. Each scapula was observed to see the presence of completely ossified STSL. Representative photograph of STSL were taken using digital camera (sony 16 megapixel).Quantative data pertaining to the dimensions of STSL were recorded in milimeters.Dimensions of STSL (Superior maximal length, inferior maximal length, thickness at medial and lateral end) has been measured with divider and meter scale. The scapula with bilaterally damaged superior margin were excluded from the study.
RESULTS
Macroscopic examination revealed that 8 (3- right side, 5- left side) out of 131 (6.1%) scapulae had completely ossified STSL.Dimensions measuredare given in Table-2.
DISCUSSION
Thecompletely ossified STSL is one of the most important factorsof suprascapularnerve entrapment neuropathy andmay pose achallengeat surgical exploration during a suprascapular nerve decompression.6,12Incidence of complete ossification of STSL differs from population to population as shown in table-1. In the present study we observed 6.1% incidence of completely ossified STSL which is close to Polguej12( 6.25%).Silva etal. 13 have reported 30.76% incidencewhich is quite high as compared to our study(6.1%).Gray D J14 found 6.34%(73 in 1151) suprascapular foramen but no foramen in 87 Indian scapulae. In some population complete ossification of STSL was very rare for eg. in Alaskan Eskimos-0.3%, native American- 2.1- 2.9%.15Osuagwuet al. 10 reported a case of complete ossification of STSL in Nigerian male adult. Khan16andDas etal. 17also have reported cases of complete ossification of STSL in Indian population.Cohen18et al described a familial case of calcification of STSL affecting a 58 year old man and his son who had STSL calcification causing entrapment neuropathy of suprascapular nerve and its attendant clinical symptoms of pain, weakness and atrophy of supraspinatus muscle. Usually cases of Suprascapular nerve entrapment neuropathy due to ossified STSL complain of deep and diffuse, poorly localized dullor burning pain in the posterolateralaspectof shoulder, which exaggerate on activity and often can be elicited by palpation over the region of the scapular notch. In some cases the pain radiates to theipsilateral extremity, the side of the neck or the front of the chest. The pain is accompanied by weakness on abduction and external rotation of the shoulder and atrophy of supraspinatus and infraspinatus muscle.19,20Muscle atrophy usually begins before the clinical signs andsymptoms and patient’s complaints.19,20,21Thethorough understanding of anatomy of suprascapular nerve is of paramount importancefor an early diagnosis and proper treatment. Suprascapular nerve, a long mixedsensorimotor peripheral nerve originates from the lateral aspect of superior trunk of the brachial plexus with contribution from the 5th and 6th anterior cervical roots, occasionally from 4th root as well. The nerve then travelsdown to reach the upper border of the scapula and enters the supraspinatus fossa through the suprascapular notchbelowthe STSL(suprascapular vessels usually abovethe STSL). The nerve travel obliquely along the floor of the supraspinatus fossa under supraspinatus muscle,supplies it and take a sharp turn around the lateral margin of the base of the scapular spine with the suprascapular vessels passing below a debated(60.8%)22spinoglenoid ligament to enter the infraspinatus fossa.Here it supplies the infraspinatus muscle.1,4,5,11,19,23 The suprascapular nerveentrapment neuropathy may be of -chronic type (compression, traction, friction leading to repetitivemicrotrauma) or acute type (direct trauma eg. fracture of scapula,dislocation of shoulder,fractureneck of humerus,fracture of the clavicle).11,20,21Suprascapular nerve is commonly susceptible to compression mainly at two major sites, suprascapular notch and spinoglenoid notch.6 Suprascapular nerve injury at suprascapular notch may occur as a result of compression by the overlying superior transverse scapular ligament, specially if it is ossified,12,17 calcified,18 bifid,24 trifid,6 hypertrophied25and/or presence of anterior coracoscapular ligament just below the STSL as reported by Avery 60% (16 in 27)26, Bayramoglu18.8%(6 in 32 )23 , Piyawinijwong 28%(19 in 127)27, Polguej50%(47 in 93)12 and/or presence of space occupying lesion eg. ganglionic cyst reported by Ticker6 , might be due to reduction in available space for the suprascapular nerve passage. The shape of suprascapular notch has been associated with the risk of nerve injury as well. Rangachary9 et al. examined 211 cadaveric scapulae and categorized the notch shape into 6 different types –TypeI-no discrete notch, Type IIwide V-shaped notch, TypeIII- wide U-shaped notch, TypeIV- narrow V-shaped notch with impression of nerve, TypeV- U-shaped notch with partial ossification, TypeVI- bony foramen.Our study is concerned to Type VI. Ticker6 classified the notch into two types ‘U’and ‘V’shaped. Although it has been hypothesized that suprascapular nerve entrapment is more likely to be associated with narrow V-shaped notch, no direct correlation between notch type and suprascapular nerve injury has been demonstrated.28 The suprascapular nerve entrapment neuropathywithout visible ossification of STSLcan be explained by another mechanism of nerve injury ie. traction (mechanical stretching) with or without friction (rubbing) of suprascapular nerve. The nerve courses through several areas of critical nerve fixation (like at the site of emergence and termination of the nerve, at the suprascapular notch and spinoglenoid notch, on the floor of supraspinatus fossa under the hypertrophied supraspinatus muscle) and areas of sharp turns. Due to repetitive overhead activities and forceful rotational movements during sports such as volleyball,29baseball,30the suprascapular nerve is subjected to traction and kinking specially at suprascapular and spinoglenoid notches as the nerve is within a notch and held by a overlying ligament.6,24,25,31Rangachary9 et al. found that nerve become closely opposed to the STSL with depression, retraction and hyperabduction of shoulder and hypothesized that mechanism of nerve injury might involve kinking of the nerve against the STSL(sling effect). The stretching of the nerve may also be exacerbated by scapular protraction which move the scapula(and its base of the spine) laterally. It has been hypothesized that this stretching of nerve can be further exacerbated by simultaneous contraction of infraspinatus muscle in which contracted infraspinatus muscle pulls the nerve medially while it is tethered laterally by the base of the spine of the scapula.29 It has been shown that spinoglenoid ligament inserts into posterior glenohumeral capsule, so during cross body adduction and internal rotation, ligament is tightened and nerve is compressed.22,32Sandowet al. reported that during extreme abduction and full external rotation medial tendinous margin of the supraspinatus and infraspinatus can impinge strongly against the lateral edge of spine, compressing the infraspinatus branch of suprascapular nerve.33Hypertrophied spinoglenoid ligament also causes compression of suprascapular nerve at spinoglenoid notch leading to suprascapular nerve entrapment neuropathy as described by Aeilloet al32. Most paralabral cysts compress the suprascapular nerve only at spinoglenoid notch as it passes within 21 mm from the glenoid rim.34The enlarged spinoglenoid notch vein has been identified as cause of suprascapular nerve compression.35 Another hypothesis of injury is that the intimal damage of axillary or suprascapular artery due to direct trauma or friction can result in microemboli of the vasa nervorum which can result in ischaemic injury to the nerve.31 The best method to prevent permanent muscle atrophy is the early diagnosis and treatment.While dealing a case of shoulder pain and weakness, along with the natural history of suprascapular nerve injury, family history of such complaints and related treatment should be taken into consideration which may help in diagnosis.Most of the authors have agreed that electromyography(EMG) study is essential to confirm suprascapular nerve entrapment neuropathy. The nerve conduction velocity(NCV) is helpful but not essential for the diagnosis.19Radiograph and CT-scan may be useful in assessing the shape of notch, calcified ligament or fracture callus. MRI is particularly helpful in identifying course of nerve, presence of soft tissue lesion(usually cyst) and also in ruling out the other causes of shoulder pain such as rotator cuff tear.20,21 The treatment of suprascapular entrapment neuropathy depends on the duration of the symptoms and the location and cause of entrapment.36If the neuropathy is of acute onset or secondary to a traction injury rather than to a compressive neuropathy, it should respond to non-operative treatment consisting of relative rest and pain control followed by progressive range of motion and controlled strengthening excercises. However, residual atrophy may persist regardless of the type of treatment.21,37If the nerve lesion is proximal and both the supraspinatus and infraspinatus muscles are involved, the entire nerve should be decompressed but most importantly the superior transverse scapular ligament should be released or sectioned from its medial attachment to minimize the risk of injury to the more laterally located suprascapular nerve and vessels.21The ossified STSL is a relative contraindication to the arthroscopic release of STSL.So it should be evaluated preoperatively when considering arthroscopic neurolysis.37 A quarter-inch osteotomy can be used to resectthe ossified STSL.38But if only the infraspinatus muscle is involved or there is a structural lesion at the spinoglenoid notch such as paralabral cyst, the nerve may be simply decompressed at the notch. Some surgeons recommend release or section of both the suprascapular and spinoglenoid ligaments even if lesion is at spinoglenoid notch.20,34Surgical exploration withrelease of compression or traction does not help in regeneration of the nerve or resolution of the atrophy.21 Limitation of the study is that the person with ossified STSL might have suprascapularnerve entrapment neuropathy,but the work was done on dry bone so without clinical history it is hard to say that person had suprascapular nerve entrapment neuropathy.Since the present study was performed with a limited number of dry scapulae,more clinical, radiological and cadaveric studies need to be done.
CONCLUSIONS
The present study revealed that incidence of complete ossification of STSL varied in different populations and it can be one of the risk factors for suprascapular entrapment neuropathy.The anatomical knowledge of understanding of the mechanism of this neuropathy may be helpful in planning the appropriate treatment strategy and thus avoiding the poor treatment outcome or treatment failure.
ACKNOWLEDGEMENT
We sincerely thank the Department of Anatomy, SVS Medical College, Mahabubnagar, Andhra Pradesh and Raichur Institute of Medical Sciences, Raichur, Karnataka for granting permission to carry out the work. Authorsalso acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript.
References:
1. Standring S, ed. Gray’s Anatomy. 40th Ed., New York, Churchill Livingstone. 2008; 794-821.
2. Stedman’s Medical Dictionary.28th ed. Julie K. Stegmans: Lippincott Williams and Wilkins; 2006. Superior transverse scapular ligament; pg-1090.
3. B. Moriggl, P. Jax, S. Milz, A. Buttner and M. Benjamin.Fibrocartilage at the entheses of the suprascapular (superior transverse scapular) ligament of man-a ligament spanning two regions of a single bone. J. Anat. 2001;199, pp. 539-545,
4. Gelmers and Buys. Suprascapular entrapment neuropathy. ActaNeurochirurgica1977;38,121-124.
5. Yang HJ,GilYC,JinJD,Ahn SV, Lee HY.Topographical anatomy of the suprascapular nerve and vessels at the suprascapular notch.Clin Anat.2012 Apr;25(3):359-65.
6. Ticker, J. B.; Djurasovic, M.; Strauch, R. J.; April, E.W.; Pollock, R. G.; Flatow, E. L. andBigliani, L.U. The incidence of ganglion cysts and variations in anatomy along the course of the suprascapular nerve. J. Shoulder Elbow Surg., 1998;7(5):472-8.
7. Harris, R. I.; Vu, D. H.; Sonnabend, D. H.; Goldberg, J. A. and Walsh, W.R. Anatomic variance of the coracoclavicular ligaments. J. Shoulder Elbow Surg., 2001;10:585-8.
8. Dunkelgrun M, Iesaka K, Park SS,Kummer FJ, and Zuckerman JD. Interobserver reliability and intraobserver reproducibility in suprascapular notch typing. Bull Hosp Joint Dis.2003;61:118-22.
9. Rengachary, S. S.; Burr, D.; Lucas, S.; Hassanein, K.M.; Mohn, M.P. andMatzke, H. Suprascapular entrapment neuropathy: a clinical, anatomical, and comparative study. Part 2. Anatomical study. Neurosurg.,1979;5:447-51.
10. Osuagwu, F. C; Inocemi, I. O. andShokunbi, M. T. Complete ossification of the superior transverse scapular ligament in a Nigerian male adult. Int. J. Morphol., 2005;23(2):121- 2.
11. Holzgraefe M, Kukowski B, Eggert S. Prevalence of latent and manifest suprascapular neuropathy in high level volleyball players. Br J Sports Med. 1994;28:177-179.
12. Michal Polguj, Jedrzejewski K, AgataMajos, Topol M. Variations in bifid superior transverse scapular ligament as a possible factor of suprascapular entrapment: an anatomical study. Int. Ortho. (SICOT). 2012;36:2095-2100.
13. Silva, J. G.; Abidu-Figueiredo, M.; Fernandes, R. M. P.; Aureliano-Rafael, F.; Sgrott, E. A.; Silva, S. F. and Babinski, M. A. High Incidence of Complete Ossification of the Superior Transverse Scapular Ligament in Brazilians and its Clinical Implications Int. J. Morphol., 2007;25(4):855-859.
14. Gray, D. J. Variations in the human scapulae. Am. J. Phys. Anthropol., 1942;29:57-72.
15. Hrdlicka A. The scapula: visual observations. Am J PhysAnthropol. 1942;29:73-94.
16. Khan, M. A. Complete ossification of the superior transverse scapular ligament in an Indian male adult. Int. J. Morphol.,2006;24(2):195-6.
17. Srijit Das, Rajesh Suri,VijayKapur. Ossification of Superior Transverse Scapular Ligament and its Clinical Implications. Sultan Qaboos University Medical Journal. August 2007 ;Vol 7, No. 2, P. 157-160 .
18. Cohen, S. B.; Dnes,D.M.and Moorman, C.T. Familial calcification of the superior transverse scapula ligament causing neuropathy. Clin. Orthop. Rel. Res., 1997;334:131-5.
19. Martin SD, Warren RF, Martin TL, Kennedy K, O’Brien SJ, Wickiewicz TL. Suprascapular neuropathy: results of nonoperative treatment. J Bone Joint SurgAm. 1997;79:1159-1165.
20. Th. Fabre, C. Piton, G. Leclouerec, F. Gervais-Delion, A. Durandeau Entrapment of the suprascapular nerve J Bone Joint Surg Br.,May 1999;Vol. 81-B, No. 3, 414-419.
21. Marc R Safran Nerve Injury About the Shoulder in Athletes, Part 1 Suprascapular Nerve and Axillary Nerve .The American J of Sports Medicine, 2004;Vol. 32, No. 3 , 803-819.
22. Demirhan M, Imhoff AB, Debski RE, Patel PR, Fu FH, Woo SL The spinoglenoid ligament and its relationship to the suprascapular nerve. J Shoulder Elbow Surg. 1998 May-Jun;7(3):238-43.
23. A. Bayramoglu, D. Demiryurek, E. Tuccar, M. Erbil, M.M. Aldur, O. Tetik, M.N.Doral. Variations in anatomy at the suprascapular notch possibly causing suprascapular nerve entrapment: an anatomical study. Knee Surg Sports Traumatol Arthrosc,2003;11:393- 398.
24. Alon M, Weiss S, Fishel B, Dekel S. Bilateral Suprascapular nerve entrapment syndrome due to an anomalous transverse scapular ligament. ClinOrthop. 1988;234:31-33. 25. Garcia G, McQueen D. Bilateral suprascapular nerve entrapment syndrome: case report and review of the literature. J Bone Joint Surg Am. 1981;63:491-492.
26. Avery BW, Pilon FM, Barclay JK. Anterior coracoscapular ligament and suprascapular nerve entrapment. Clin Anat. 2002;15:383- 386.
27. PiyawinijwongSithaPiyawinijwong, PhongpanTantipoon, The Anterior Coracoscapular Ligament in Thais: Possible Etiological Factor of Suprascapular Nerve Entrapment .Siriraj Med J 2012; 64 (Suppl 1): S12-S14.
28. Cummins CA, Anderson K, Bown M, Nuber G, Roth SI. Anatomy and histological characteristics of the spinoglenoid ligament. J Bone Joint Surg Am. 1998;80:1622-1625.
29. Ferretti A, Cerullo G, Russo G. Suprascapular neuropathy in volleyball players. J Bone Joint Surg Am. 1987;69:260-263.
30. Bryan WJ, Wild JJ Jr. Isolated infraspinatus atrophy. A common cause of posterior shoulder pain and weakness in throwing athletes? Am J Sports Med 1989;17:130-1.
31. Ringel SP, Treihaft M, Carry M, Fisher R, Jacobs P. Suprascapular neuropathy in pitchers. Am J Sports Med. 1990;18:80-86.
32. Aiello L, Serra G, Traina GC, Tugnoli HW. Entrapment of the suprascapular nerve at the spinoglenoid notch. Ann Neurol. 1982;12:314- 316.
33. Sandow MJ, Ilic J. Suprascapular nerve rotator cuff compression syndrome in volleyball players. J Shoulder Elbow Surg. 1998;7:516-521.
34. Fehrman DA, Orwin JF, Jennings RM. Suprascapular nerve entrapment by ganglion cysts: a report of six cases with arthroscopic findings and review of the literature. Arthroscopy. 1995;11:727-734.
35. Carroll KW, Helms CA, Otte MT, Moellken SMC, Fritz R. Enlarged spinoglenoid notch veins causing suprascapular nerve compression. Skeletal Radiol.2003;32:72- 77.
36. Sarah yanny, Andoni P. Toms. MR patterns of denervation around the shoulder. Musculoskeletal Imaging Review. AJR:195, August 2010.
37. Peter J. Millett, R. Shane Barton, Iva´n H. Pacheco and Reuben Gobezie. Suprascapular Nerve Entrapment: Technique for Arthroscopic Release Techniques in Shoulder and Elbow Surgery2006;7(2):1-6.
38. Ghodadra Neil Ghodadra, M.D., Shane J. Nho, M.D., M.S., Nikhil N. Verma, M.D., StfanieReiff, B.A.,Dana P. Piasecki, M.D., Matthew T. Provencher, M.D., and Anthony A. Romeo, M.D. Arthroscopic Decompression of the Suprascapular Nerve at the Spinoglenoid Notch and Suprascapular Notch Through the Subacromial Space. Arthroscopy: The Journal of Arthroscopic and Related Surgery,April 2009;Vol.25 No 4, 439-445.
39. Natsis K, Totlis T, Tsikaras P, Appell HJ, Skandalakis P, Koebke J. Proposal for classification of the suprascapular notch: a study on 423 dried scapulas. Clin Anat. 2007;20:135–9.
40. Edelson JG. Bony bridges and other variations of the suprascapular notch. J Bone Joint Surg Br. 1995;77:505–6.
41. Sinkeet SR, Awori KO, Odula PO, Ogeng’o JA, Mwachaka PM. The suprascapular notch: its morphology and distance from the glenoid cavity in a Kenyan population. Folia Morphol (Warsz). 2010;69:241–5.
42. S D Jadhav, R J Patil, P P Roy, M P Ambali, M A Doshi, Rajeev R Desai Supra-scapular foramen in Indian dry scapulae. National Journal of Clinical Anatomy. 2012 Vol.- 1(3), 133-135.
43. KalpanaThounaojam, RenucaKaram, N. Saratchandra Singh. Ossification of transverse scapular ligament. Journal of Evolution of Medical and Dental Sciences. 2013;Vol-2(12):1790-91.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License