IJCRR - 9(11), June, 2017
Pages: 24-29
Date of Publication: 12-Jun-2017
Print Article
Download XML Download PDF
Needle Stick Injury: A Study Among Interns and Post Graduate Scholars at a Tertiary Level Care Hospital
Author: Shakeel Ahmad, Abdul Ghani, Aamir Yaqoob, Omeshwar Singh
Category: Healthcare
Abstract:Introduction: Needle stick injury is an underestimated problem among health care personnel all over the world.More than 20 types of blood borne pathogens especially Hepatitis B virus, Hepatitis C virus and Human immune deficiency (HIV) virus can be transmitted through needle stick injuries.
Aim of Study: The main aim of our study was to assess awareness regarding needle stick injuries with risk of serious infections and awareness regarding first aid and post exposure prophylaxis.
Material andMethods: Data was collected in the form of pre-tested self-administered questionnaire. 100 students participated in the study. The response to questionnaire was analysed and results were obtained.
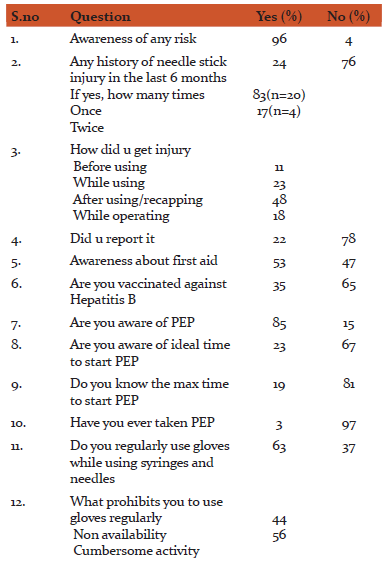
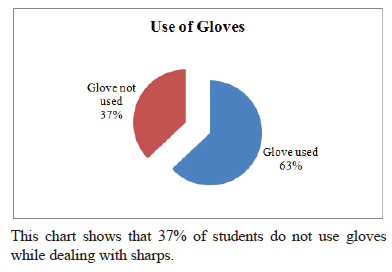
Results: The incidence of needle stick injury among students was found to be 24%.47% of students were not aware of recommended first aid after needle or sharp injury.Regarding Hepatitis B vaccination, 65% were not vaccinated, only 35% were vaccinated. 94% of students had never received any training regarding sharps.
Conclusion: This study showed a high rate of needle stick injuries among interns and post graduate students. Still the incidence is on lower side, owing to non-reporting of injuries. The strong predictor for needle stick injury was lack of training and work load. Recapping of needles was found to be the most common reason for needle stick injuries.
Keywords: Needle sticks injury, Hepatitis B virus, HIV, Interns, PEP
Full Text:
INTRODUCTION
Needle stick Injury is an inevitable event for hospital staff involved in patient care at a health care facility. The medical profession carries a disproportionate burden of significant exposures (i.e. exposure to a high-risk patient). The risk is profound among medical studentsdue to lack of experience and protective measures being offered at a govt. hospital in a developing country. More than 20 types of blood borne pathogens especially Hepatitis B virus, Hepatitis C virus and Human immune deficiency (HIV) virus can be transmitted through needle stick injuries1, 2. The estimated risk of acquiring HIV infection after percutaneous exposure to blood from an HIV-infected patient is 0.3 percent3. According to the United States National Institute for Occupational Safety and Health (NIOSH), Needle stick injuries are injuries caused by needles such as hypodermic needles, blood collection needles, sterile intravenous needles etc4.The activities associated with the majority of needle stick injuries are administering injections, withdrawing blood, recapping needles, disposing off needles, handling trash and dirty linen and missing the target while attempting to transfer blood or any other body fluid from a syringe to a specimen container5, 6.
Economic costs imposed by the treatment and the consequent stress are the other complications of sharp injuries7. Job stress during performing duty is reported to be a contributory factor in this regard8.
The prevalence of blood-borne viruses such as Hepatitis B, Hepatitis C and Human immune deficiency virus (HIV) continue to increase in the general community9, 10. Trend data collected by the Health Protection Agency Centre for Infection Surveillance between 2002 and 2005, reported in The Eye of the Needle11, revealed a 49% overall increase in reported occupational exposures among U.K surgeons.
Due to underreporting, the incidence of sharp injury has been underestimated; although sharps injuries are one of the most common types of injury incurred by health care workers and the consequences to those involved may be catastrophic. It is apparent that current surgical practice has the potential to leave the healthcare worker exposed.
Only a few studies have been published on needle stick injuries from this area or from developing countries in general; although 90% of needle stick injuries occur in developing countries12.
In India, relatively few studies have addressed the issue of needle stick injury among medical students. Our study mainly focuses on calculating the incidence, identifying risk factors and awareness about needle stick injury and about precautionary measures and post exposure prophylaxis(PEP) being offered at a govt. hospital.
AIM OF STUDY
The aim of this study was to:
- To study about awareness of any risk associated with needle or sharp injury andpost exposure prophylaxis.
- To establish the true incidence of needle-stick injury among medical students; and
- To assess the knowledge of universal precautions, risk perception of needle stick injury among medical students.
MATERIALS AND METHODS
Our study is a cross-sectional study conducted in 2014- 2015 at Govt medical collegeJammu. The study was conducted among interns and post graduate students.100 students participatedin our study.All the participants were explained the objective of the study and written informed consent was taken from each of them
Inclusion criteria
Being working as intern and postgraduate student for more than 6 months
The consent to participate in thestudy
Exclusion criteria
Interns and medical students with less than 6 months of practice at themoment
Lack of cooperation and proper completion of the questionnaire
Data was collected in the form of pre-tested self-administered questionnaires as depicted below. The pre-tested structured questionnaire was distributed to all the students. The questionnaire included characteristics related to the study (cause of the incident, time of incident, injured member and cause of injury) and sectionrelated to the explanation of how the incident had happened. The confidentiality of information was explained to the students. They were assured thatthe information was going be used in a research work.
QUESTIONAIRRE
DESIGNATION:SPECIALITY:
- Are you aware of any risk associated with needle or sharp injury? (yes/no)
- Did you have any needle stick injury or needle prick in last 6 months? (yes/no)
- How many times.
- How did you get the needle prick? (before/while/afterusing or while operating)
- Did you report it?
- Are you aware of any recommended first aid after needle or sharp injury?
- Are you vaccinated against Hepatitis B? (no, partial, full)
- Are you aware of post exposure prophylaxis (procedure, duration and place)? (yes/no)
- Are you aware of ideal time to start PEP? (yes/no)
- What is the maximum time to start prophylaxis after exposure? (know/don’t know)
- Have you ever taken PEP?
- Do you regularly use gloves while using syringes or needles?
- What prohibits you to use gloves regularly? (non availability or cumbersome activity)
- How do you dispose of the sharps?
- Have you ever received training related sharps disposal? (yes/no)
- Do you do recapping of needles? (Yes/no).
RESULTS AND OBSERVATIONS
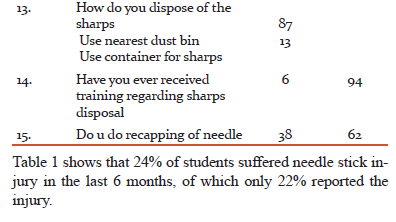
A total of 100questionnaires were distributed among interns(n = 50) and post graduate students(n = 50). The response to questionnaires was collected after 1 week. The data was analysed and the results obtained. Out of 100, 96 students were aware of risk associated with needle or sharp injury, whereas 4 students were unaware of any risk associated with sharps. The incidence of needle stick injury among students was 24%. Of these 24Needle stick injuries, 20 had injury onceand 4 students had history of injury twice. The incidence of needle stick injury was maximum while recapping of needles after use. 22% of injuries were reported while as, 78% of injuries were not reported.
47% of students were not aware of recommended first aid after needle or sharp injury. Regarding Hepatitis B vaccination, 65% were not vaccinated, only 35% were vaccinated. Only 85% of students were aware of post exposure prophylaxis (PEP), whereas 15% were not aware of PEP. Only 23% of cases were aware of ideal time to start post exposure prophylaxis. Of the students reporting needle stick injury, only 3 students had taken post exposure prophylaxis. Routinely, only 63% of students use gloves while dealing with syringes and sharps. From the study, students reported that 87% dispose off sharps in the nearest dust bin available. 94% of students had never received any training regarding sharp disposal. 38% of students would do recapping of needles after use.
DISCUSSION
Our study supports previously published work demonstrating that needle-stick injury is common and significantly an under-reported problem13, 14; also it demonstrated that students are particularly a high risk group. With the rising population prevalence of bloodborne viruses15and the increasing incidence of all exposures, we believe that the risks to the health care personnel are increasing. We propose that the students before joining the hospital should receive a proper training regarding use of sharps, their disposal, about first aid in case of needle stick injury, about PEP and Hepatitis B vaccination. While training of users will always be important in prevention, engineering and administrative controls are likely to be effective as well.
The constant use of sharps in theemergency department, wards and operation theatre creates an environment where the incidence of needle stick injury has increased to a significant extent. By establishing the true incidence of the needle stick injury, the next step is to tackle the circumstances surrounding the incidents and the subsequent post event behaviour. To do so, we must look at the on-spot decision making that goes on at the time of an incident.Also, further studies are advised to estimate the incidence and address the problem of needle stick injury properly.
Our experience and findings in this study suggest that the use of gloves is viewed as cumbersome activity while dealing with the sharps. Due to huge work load, the needle stick injury is mostly not reported.Recapping of used needles, suturing especially during long working hours and cleaning after patient care were related to higher incidence of the injuries.
We set out in this study to establish the true incidence of needle-stick injury by anonymously questioning interns and postgraduate students of all grades and specialities in our centre. The 24% who anonymously admitted to needle-stick injury over our studyis lower as compared to previously reported incidences by Chen et al16 (71.3%), Holla R et al17 (71.9%) and Maryam Amini et al18 (67.8%). This difference could be explained by the fact that our study population included only interns and postgraduates, while the other studies have included all health care workers. Some of the other studies indicated that the rates are higher for nurses than for other health care worker groups. Work by Elmiyeh et al13studying all healthcare workers showed an incidence of 38% per year. In their study, 51% of respondents reported all of their injuries. Wallis et al.25 found a mean rate of 1.4 sharps or eye exposures per year (range 0–12 exposures per year) in consultant orthopaedic surgeons with a reporting rate of 33% (their overall questionnaire response rate was 34%).
In developing countries, high patient-to-doctor ratio results in junior staff having to take on some of the senior doctors’ responsibilities e.g. carrying out minor surgical procedures. They may not be adequately trained for these and consequently are exposed to a high risk of needle stick injuries.
We feel these post-exposure response rates particularly in the intern cohort are unacceptably low. Our study is small, retrospective and confined to one centre, but we have no reason to believe that its findings are not accurate or representative of the wider problem. These under-reporting rates fall significantly short of any study reported before.
Training was found to be the crucial factor in predicting the occurrence of needle stick injuries among the interns and post graduates in our study. This finding has great importance for planning preventive measures in developing countries where arranging proper training is a more feasible target than buying expensive equipment.
Hand washing after patient contact, use of personal protective equipment such as gloves and minimization of manual manipulation of sharp instruments and devices and safe disposal of used sharp items can reduce the incidence of needle stick injuries. Use of gloves while handling sharp instruments is a precautionary measure recommended and compliance with this seemed to be an indicator for risk behaviour. Muralidhar et al20 in their study reported that majority of health care workers (74%) were wearing gloves at the time of Needle Stick Injury. Majority of orthopaedic surgeons prefer wearing double gloves to prevent hazards of needle stick injuries.
Our study showed a significantly increased risk of needle stick injuries among those who were recapping needles most or all of the time compared with those who were not recapping. This finding is consistent with earlier studies. Sharma et al19 and Muralidhar et al20 reported recapping as the most common procedure responsible for Needle Stick Injuries with 34% and 39% NSIs respectively associated with recapping. Location of the sharps containers may explain a part of this high rate of recapping needles.
Working excessive hours can result in stress and emotional and physical exhaustion which are likely to increase the chance of human error and contribute to a tendency towards high risk behaviours such as recapping needles and poor compliance with the precautions in general21. Long working hours is also an indicator of understaffing, a common phenomenon in developing countries22.
We found out that needle stick injury by a needle contaminated with a low risk patient is unlikely to raise an alarm in the mind of the treating doctor. There is a sense of security arising from the Hepatitis B vaccination. The only cases reported in The Eye of the Needle where Hepatitis B transmission had occurred in healthcare workers who were not immunised or only mounted a partial response to the vaccine11. Furthermore, HIV post-exposure prophylaxis using anti-retroviral agents is unpleasant and not without its own risks. We doubt, however, that any surgeon would question the benefits of post-exposure prophylaxis following a known transmission. For Hepatitis C, there is no effective post-exposure prophylaxis currently available.
We also postulate that each hospital should establish a centre, where these needle stick injuries would be reported immediately by the health care personnel and necessary action being taken to prevent catastrophic consequences on the sufferer. The reporting system should be kept simple. The main reasons behind non-reporting of cases was the lack of knowledge, how to report the needle stick injury. Other factors implicated are very low risk patient, afraid of a positive result which may affect career13.
In a study by Jagger et al, disposable syringes accounted for 35 percent, intravenous tubing and needle assemblies for 26 percent, prefilled cartridge syringes for 12 percent, winged steel-needle intravenous sets for 7 percent, phlebotomy needles for 5 percent, intravenous catheter stylets for 2 percent, and other devices for 13 percent. Devices that required disassembly had rates of injury of up to 5.3 times the rate for disposable syringes23.
Testing of the source blood allows the surgeon to receive post-exposure prophylaxis for as short a period as possible, a full course in the event of a HIV exposure or follow-up with a view to early treatment when indicated following a Hepatitis C exposure. If the source is found to be without blood-borne infections, the post-exposure prophylaxis can usually be stopped after a short period (24–48 h). In a study by Anjum et al24on needle stick injuries, majority (92.6%) of employees immediately washed the exposed part, 5% of the employees washed exposed part, reported to the authorities and took PEP while as a small percentage 0.5% took only PEP.
Lastly, we suspect that surgeon apathy and other perceived priorities cause significant under-reporting. Wallis et al25found that the most common reason for not reporting exposures by orthopaedic consultants was that the reporting system was too complex.
CONCLUSION
- The hospital administration has a duty to provide a safe environment, to create awareness and educate all medical students about the risk of viral transmission and PEP and to enforce reporting of all incidents.
- Recapping of needles should be discouraged and sharp containers should be provided in each ward.
- Practice safe use of sharps and adhere to recommended guidelines while using sharps.
- Post-exposure tests must be made readily available in all the hospitals. Post Exposure Prophylaxis should be readily made available as well.
- Use of gloves preferably double gloves should be strictly followed.
- Hepatitis B vaccination should be provided free to all the staff working in the hospital. The procedure should be repeated every year to provide vaccination to fresh candidates.
Acknowledgement
We are thankful to all those students of the institute who participated in the study. Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Ethical Clearance:Taken
Informed Consent:Taken individually
Financial support:Nil
Conflict of interest: Nil
References:
- Yang YH, Liou SH, Chen CJ, Yang CY, Wang CL, Chen CY, Wu TN. The effectiveness of a training program on reducing needle stick injury among graduate vocational nursing school student’s southern Taiwan. Journal of Occup Health. 2007; 49:424-9.
- Hasselhorn HM. The hepatitis B, hepatitis C or HIV infectious health care workers. In: Hasselhorn HM, Toomingsas A, Lagerstrom M (Eds). Occupational health for health care workers: a practice guide. The Netherlands: Elsevier Science. 1999; 44-9.
- Heptonstall J, Porter K, Gill ON. Occupational transmission of HIV: summary of published reports — December 1995. London: Public Health Laboratory Service, Communicable Disease Surveillance Centre, 1995.
- C Doig: Education of medical student and house staff to prevent hazardous occupational exposure. CMAJ. 2000; 162, 344-345.
- C Shen, J Jagger and RD Pearson. Risk of needle stick and sharp object injuries among medical students. Am J Infect control 27, 435 – 437(1999).
- OSHA. Safer needle devices: protecting health care workers, 1997. (Online). http://www.thebody.org/osha/saferneedle/02.html(20January 2002).
- Zanni, G. R., and Wick, J. Y. (2007). Preventing needlestick injuries. The Consultant Pharmacist, 22(5), 400-409. http://dx.doi.org/10.4140/TCP.n.2007.400.
- Makary, M. A., Al-Attar, A., Holzmueller, C. G., Sexton, J. B., Syin, D., Gilson, M. M., Sulkowski, M. S., and Pronovost, P. J. (2007). Needle sticks injuries among surgeons in training. New England Journal of Medicine,356(26): 2693-2699. http://dx.doi.org/10.1056/NEJMoa070378.
- Health protection agency. Shooting Up. Infection among drug users in the United Kingdom 2006, an update: October 2007. http://www.hpa.org.uk/infections/topics_az/injectingdrugusers/shooting_up.htm.
- Health protection agency. Testing limes HIV and Sexually Transmitted Infections in the United Kingdom 2007; http://www.hpa.org.uk/infections/topics_az/hiv_and_sti/publications/AnnualReport/2007/default.htm.
- Health Protection Agency. Eye of the Needle, United Kingdom Surveillance of Significant Occupational Exposures to Blood-borne Viruses in Healthcare Workers 2006;http://www.hpa.org.uk/publications/PublicationDisplay.asp?PublicationlD=54.
- World Health Organization (WHO), Safe Injection Global Network (2003) Health Care Workers Safety. Aide-Memoire for a Strategy to Protect Health Care Workers from Infection with Blood Borne Viruses. WHO/BCT/03.11, 2003.
- Elmiyeh B, Whitaker IS, James MJ, Chahal CA, Galea A, Alshafi K. Needle-stick injuries in the National Health Service: a culture of silence. J R Soc Med 2004; 97: 326–7.
- Debnath D. Improving reporting of sharp injuries. Hosp Med 2000; 61: 852 – 4.
- Sharps safety policy, Royal United Hospital Bath, Ref No 619 2006, ratified September2006.http://www.ruh.nhs.uk/documents/trustpolicies/yellow_infectioncontrolpolicies/Yellow6192006SharpsSafetyPolicy.doo>
- Chen L, Zhang M, YanY, MiaoJ, Lin H, ZhangY, et al. Sharp object injuries among health care workers in a Chinese Province. AAOHN J.2009;57(1):13-16.
- Holla R, Unikrishnan B, Ram P, Thapar R, Mithra P, Kumar N et al. Occupational exposure to needle stick injuries among health care personnel in a tertiary care hospital: A cross sectional study. J. Community Med Health Education S2:004.doi:10.4172/2161- 0711,S2-004.
- Amini M, Behzadnia MJ, Saboori F, Bahadori MK, Ravangard R. Needle stick injuries among health care works in a Teaching Hospital. Trauma Monthly. 2015 Nov;20(4).
- Sharma R, Rasania SK, Verma A and Singh S. Study of prevalence and response to needlestick injuries among health care workers in a tertiary care hospital in Delhi, India. Indian J Community Med 2010;35(1):74-77.
- Muralidhar S, Singh PK, Jain RK, Malhotra M and Bala M. Needle stick injuries among health care workers in a tertiary care hospital of India. Indian J Med Res 131, March 2010:405-410.
- Grosch JW, Gershon RR, Murphy LR and DeJoy DM (1999) Safety climate dimensions associated with occupational exposure to blood borne pathogens in nurses. American Journal of Industrial Medicine Supplement 1, 122–124.
- Porta C, Handelman E and McGovern P (1999) Needle stick injuries among health care workers. A literature review. AAOHN Journal 47, 237–244
- Janine Jagger, Ella H. Hunt, and Richard D. Pearson, M.D.: Rates of Needle-Stick Injury Caused by Various Devices in a University Hospital(Aug 1988). N Engl J Med 1988; 319:284-288.
- Anjum B. Fazili, Rohul J. Shah, Qazi M. Iqbal, Feroz A. Wani. Occupational Exposure and Needlestick Injuries among Employees of a Tertiary Care Institute in Kashmir. Int J Cur Res Rev | Vol 9 • Issue 7 • April 2017: 44 – 48.
- Wallis GC, Kim WY, Chaudhary BR, Henderson JJ. Perceptions of orthopaedic surgeons regarding hepatitis C viral transmission: a questionnaire survey. Ann R Coll Surg Engl 2007; 89: 276–80.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License