IJCRR - Vol 09 issue 10 current issue , May, 2017
Pages: 49-52
Date of Publication: 27-May-2017
Print Article
Download XML Download PDF
Prevalence of Asymptomatic Peripheral Vascular Disease Among Type 2 Diabetes Mellitus Patients
Author: Surendra Kumar, Akhil Gupta, Vinod Aswal, Prabhu Dayal Barala
Category: Healthcare
Abstract:Background: Peripheral vascular disease (PVD) is one of the significant Macrovascular complications of type 2 diabetes mellitus presenting commonly with symptoms of intermittent claudication, it is the leading cause for limb gangrene and hence amputation in diabetic patients, it is also accompanied by a high likelihood for symptomatic cardiovascular and cerebrovascular disease, The routine PVD assessment in type 2 DM patients showing importance in the light of a long duration of asymptomatic period in the natural course of the disease
Aim: This study was done with the aim to determine the prevalence of asymptomatic PVD among Type 2 diabetes patients, so that by early recognition of PVD, related complications can be limited
Material and Method: Our study was conducted in the Department of Medicine, S.P. Medical College and Associated group of hospitals, Bikaner. A total of 108 type-2 DM cases who visited medical outdoor and those admitted in PBM hospital were selected for study after obtaining proper informed consent
Result and Conclusion: Prevalence of asymptomatic PVD (ABI < 0.9) is about 12% in our study. Thus a significant proportion of type 2 diabetic subjects are affected by PVD, and hence due importance to be given for active screening annually specially by ABI and prevention and management of complication among type 2 diabetes patients.
Keywords: Peripheral Vascular Disease, Ankle Brachial Index, Type 2 Diabetes Mellitus
Full Text:
INTRODUCTION
Peripheral vascular disease (PVD) is one of the significant Macrovascular complications of type 2 diabetes mellitus. The most common symptom of PVD is intermittent claudication, defined as pain, cramping, or aching in the calves, thighs, or buttocks that appears reproducibly with walking exercise and is relieved by rest. More extreme presentations of PVD include rest pain, tissue loss, or gangrene; these limb-threatening manifestations of PVD are collectively termed critical limb ischemia (CLI). and while it is a major risk factor for lower-extremity amputation, it is also accompanied by a high likelihood for symptomatic cardiovascular and cerebrovascular disease15. The routine PVD assessment in type 2 DM patients showing importance in the light of a long duration of asymptomatic period in the natural course of the disease and hence the importance of active screening for PVD with special emphasis on ankle – Brachial index gains importance for saving the limbs of Diabetic patients1. Although Diabetic Peripheral Neuropathy and Peripheral Vascular Disease (PVD) both contribute to the development of diabetic foot, the risk of amputation raises steeply only if there is associated PVD2. Diabetes predominately leads to PVD in the infrageniculate arteries of calf and the risk factors associated with development of PVD in diabetes are found to be advancing age, uncontrolled hyperglycemia, hypertension, dyslipidaemia and smoking3,9.
Several population studies have shown that diabetes is a strong risk factor for PVD4 and PVD was found in approximately 20% of the diabetic patients5 but this probably greatly underestimates the prevalence, given that many more people with PVD are asymptomatic rather than symptomatic. In the United Kingdom prospective diabetes study (UKPDS) PVD was found in 11% of patients after a follow up period of 6 years from the time of diagnosis of type 2 diabetes6. It can be safely concluded based on these population studies that PVD is a highly prevalent disorder, in particular in the elderly diabetic patient. Unfortunately, the awareness of the physicians that these patients have PVD is low, resulting in inadequate preventive measures for reducing lower extremity amputation and to reduce the grossly elevated general cardiovascular risk7,8.
AIMS AND OBJECTIVES
To determine the prevalence of asymptomatic PVD among Type 2 diabetes patients, so that early recognition of PVD by active screening in diabetic subjects can be done, before devastating complications of peripheral limb ischemia develops and timely management can be done.
MATERIAL AND METHODS
Our study was conducted in the Department of Medicine, S.P. Medical College and Associated group of hospitals, Bikaner. A total of 108 type-2 DM cases who visited medical outdoor and those admitted in PBM hospital were selected for study after obtaining proper informed consent.
The exclusion criteria used were
- Clinical evidence of thromboangitisobliterans.
- Suspected arteritis subjects.
- Patients suffering from hypercoagulable states including heamotologic diseases.
- Hypothyroidism
- Collagen vascular disorders
- Valvular heart disease
- A patient without clinical evidence of coronary, cerebrovascular, and peripheral artery disease (PAD).
Present study was conducted on patients of type 2 diabetes mellitus and was interviewed with special attention on elicitation of history regarding symptoms of PVD, in the form of intermittent claudication, Ischemic rest pain, history of foot ulcers in the past and present. Smoking was recorded in pack-years of cigarettes smoked. Duration of diabetes since diagnosis was recorded and they were grouped accordingly.
The anthropometric measurements were recorded and the body-mass index was calculated. Waist-hip ratio was also recorded. The blood pressure was recorded in both the upper limbs and both the lower legs using the standard B.P cuff. An comprehensive physical examination was done and findings recorded. Special importance was given to foot examination. Peripheral neuropathy assessment was done using simmel-weiss monofilament testing and timed vibration sense perception recordings. Symptoms of peripheral neuropathy were also noted.
For detection of peripheral vascular disease recordings of ankle-brachial index (ABI) was recorded using the hand held Doppler probe (5-8 MHz) is positioned over the posterior tibial artery after applying the sphygmomanometer cuff over lower calf just above the ankle. The two consecutive readings were taken. Patients with ABI of <0.9 were taken as cases of PVD. In this study patients who had an ABI of >1.15 were screened with duplex color Doppler-imaging for screening for PVD.
Results
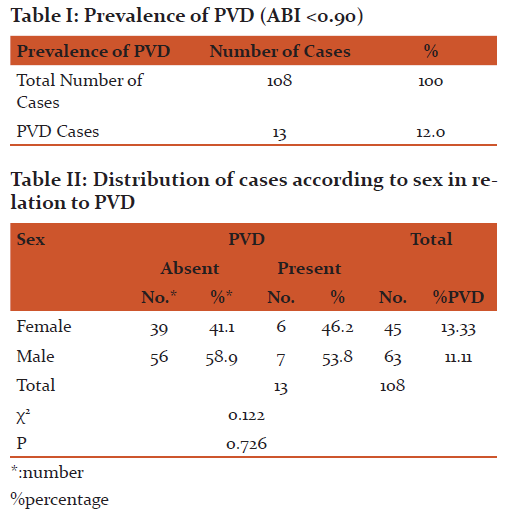
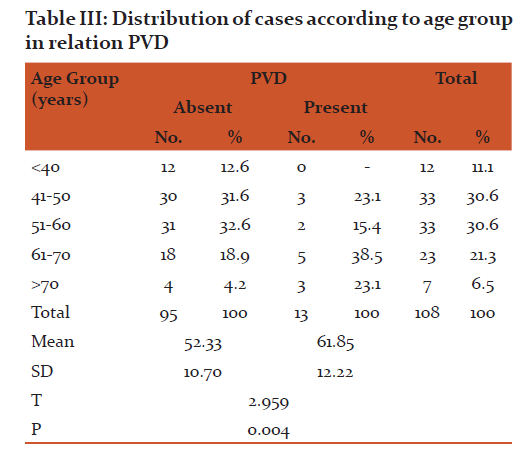
Out of total 108 patients studied 63 were males and 45 were females. Total 13 (12%) patients had PVD(peripheral vascular disease) positive, stating 12% prevalence ,which is quite significant (Table I), with women having a slightly higher prevalence (6 out of 45; 13.33%), as compared to men (7 out of 63; 11.11%).(Table II). None of the patient was symptomatic at the time of diagnosis of PVD. Mean age in PVD positive cases were 61.85±12.22 while mean age in PVD negative cases was 52.33±10.70 and the difference was found statistically significant (p<0.01)( Table III).
DISCUSSION
The importance of PVD assessment assumes importance in the light of a long duration, asymptomatic period in the natural course of the disease so the importance of active screening methods with special emphasis on ankle – Brachial index gains importance for saving the limbs of Diabetic patients10. Once there is presence of PVD in an individual, the time duration taken up for development of gross limb and life threatening sepsis after an injury is very rapid and interventions to augment peripheral blood flow during such an acute active sepsis is not possible always. Hence the importance lies in identifying the risk factors responsible for the development of PVD in type 2 diabetes, and in active screening for PVD in all diabetic subjects. Effective implementation of preventive measures in the targeted high risk group will pave the way for Limb protection.
Our study showed that prevalence and risk of development of PVD increases with age. Mean age of PVD positive cases were 61.85±12.22. Seki et al11 described that the prevalence of peripheral vascular disease (PVD) was determined in 296 Japanese diabetics (mean age 55.2 years). The prevalence of PVD was 11.11% among males and 13.33% among females in our study group. Similar trend in epidemiological studies in the year 2012 Agarwal et al 12 and in the year 1995, Mohan et al13 seen.
Mean duration of diabetes in PVD negative patients was 7.19. Mean duration of diabetes in PVD positive cases was 10.42±8.43 years while and the difference was found statistically insignificant (p>0.5).
In our study prevalence of asymptomatic peripheral vascular disease (ABI <0.90) by hand held Doppler technique was found to be 12% (13 out of 108 patients) . This high asymptomatic PVD prevalence was may be due to sedentary life, old ages unable to walk long distance and associate peripheral neuropathy, which was comparable to a study done by Meijer et al14 which showed prevalence of PVD ranging from 5.5% to 26.7%14.
CONCLUSION
Prevalence of asymptomatic (subclinical) peripheral vascular disease (ABI 0.9) is about 12% in our study. This has to be viewed seriously considering the huge type 2 diabetic population. Thus a significant proportion of type 2 diabetic subjects are affected by PVD, and hence due importance to be given for active screening annually specially by ABI and prevention and management of complication among type 2 diabetes patients.
0.9) is about 12% in our study. This has to be viewed seriously considering the huge type 2 diabetic population. Thus a significant proportion of type 2 diabetic subjects are affected by PVD, and hence due importance to be given for active screening annually specially by ABI and prevention and management of complication among type 2 diabetes patients.
Central obesity, uncontrolled hyperglycemia, hypertension, high LDL cholesterol, high triglycerides, low-HDL cholesterol and smoking are the modifiable risk factors associated with development of PVD. Advancing age was found to be the non modifiable risk factors for development of PVD.
CONFLICT OF INTEREST:
Authors declare that there is no conflict of interest
SOURCE OF FUNDING
SELF
ACKNOWLEDGEMENT:
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript, the authors are also grateful to authors editors, publishers, of all those articles, journals, and books from where the literature for this article has been reviewed and discussed.
References:
- Maedica (Buchar). 2014 Sep; 9(3): 295–302.
- Aparna Swaminathan, Vasc Health Risk Manag. 2014; 10: 417–424.
- Diabetes and cardio vascular disease – 2nd Edition Edited by Michael T. John Stone, Aristidis veves.
- Beckman JA, et al., Diabetes and athero sclerosis J AMA 2002; 287; 2570- 81.
- Macgregor A5 et al Role of Systolic – Blood Pressure and Plasma triglycerides in Diabetic peripheral arterial disease. The Edinburgh artery study. Diabetes care 1999; 22; 453-8.
- Adler AI, et al – UKPDS 59; Hyperglycaemia and other potentially modifiable risk factors for peripheral vascular disease in type 2 Diabetes melitus; Diabetes care 2002; 25; 894-9.
- Hirsch AT et al, Peripheral arterial disease detection, awareness and treatment in primary care. JAMA 2001; 286; 1317-24.
- A pelquist J et.al., what is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes metob res rev 2000; 16 (supl 1); s75-83.
- Price JF et al. Relationship between smoking and cardiovascular risk factors in the development of peripheral arterial disease and coronary artery disease; Edinburgh artery study. Eur. Heart- J 1999; 20 : 344-53.
- Beks PJ etal peripheral arterial disease in relation to glycaemic level in an elderly Caucasian population: the hoorn study. Diabetologia 1995; 38: 86-96.
- Seki J, Ohashi M, Sato T, Yamamoto M, Fujii S, Wada M. Peripheral vascular disease in Japanese diabetics: screening by the Doppler ultrasonic technique. Tohoku J Exp Med. 1983; 141 Suppl:499-506.
- Agarwal AK, Singh M, Arya V, Garg U, Singh VP, Jain V. Prevalence of peripheral arterial disease in type 2 diabetes mellitus and its correlation with coronary artery disease and its risk factors. J Assoc Physicians India. 2012; 60:28-32.
- Mohan V, Premalatha G, Sastry NG. Peripheral vascular disease in non-insulin-dependent diabetes mellitus in south India. Diabetes Res Clin Pract. 1995; 27(3):235-40.
- Meijer WT et al, peripheral arterial disease in the elderly: the Rotterdam study. Arterio sclera thromb vasc biol. 1998; 18; 185-192.
- Violi F, Atherosclerosis. 1996 Feb;120(1-2):25-35
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License