IJCRR - Vol 09 issue 10 current issue , May, 2017
Pages: 35-39
Date of Publication: 27-May-2017
Print Article
Download XML Download PDF
Uterine Arteriovenous Malformation is Rare, but Life-Threatening Disease:
A Report of 2 Cases
Author: Bakisololo Miyuna Jacqueline, Wang Huali, Mbungu Mwimba Roger, Guan Linlin
Category: Healthcare
Abstract:Aim: Though uterine arteriovenous malformation (UAVM) is a rare event, it remains a life-threatening among reproductive women. Since its original description done by Dubreuil and Loubatin 1926; approximately 100 cases have been listed in the literature.
The aim of the present report is to state the effectiveness of uterine embolization in the management of UAVM.
Case Report: In this report, we present two patients with uterine arteriovenous malformation who were admitted for recurrent vaginal hemorrhage and treated twice to thrice, prior to confirm the diagnosis. These patients had a history of either cesarean or curettage. In addition, one of the cases (case number 2) had a previous conization for cervical intraepithelial neoplasia III (CINIII) one month earlier, which is an unusual case. The diagnosis has been made by color Doppler and Spectral flow imaging (CDFI) and Digital Subtraction Angiography (DSA). One of the patients was treated with embolotherapy, while another underwent a hysterectomy. The postoperative period was favorable.
Discussion: Although the uterine embolization being effective, the treatment of UAVM is not standardized. However, it depends on the clinical condition of the patient, desire of fertility and age.
Conclusion: The uterine arteriovenous malformation is a dangerous morbidity, which requires prompt diagnosis. Doppler ultrasound and MRI are non-invasive tools for the diagnosis. Furthermore, the uterine artery angiography remains the gold procedure of the diagnosis, concomitantly leads the procedure of the embolotherapy. The embolization of the UAVM has the advantage to preserve fertility. However, hysterectomy should be considered as the last option to save the patient's life.
Keywords: Arteriovenous malformation, Cesarean, Curettage, Vaginal bleeding
Full Text:
Introduction
The arteriovenous malformation is a sporadic disease. Since its original description done by Dubreuil and Loubatin 1926[2, 12]; approximately 100 cases have been listed in the literature [1]. The UAVM accounts 1-2 % of gynecologic hemorrhage [4, 5]. In 1982, Glowacki and Milliken divided the arteriovenous malformation into two categories, congenital and acquired [8, 9].
The frequent symptom is recurrent vaginal bleeding “ex utero” [2]. Previously the diagnosis of UAVM was made by histopathology of uterine specimen after performing hysterectomy[3,7,15]. Currently, color and Spectral flow Doppler Ultrasound is the most used as well as Magnetic resonance imaging (MRI) [3, 12,14] which helps to assess the extent of the lesion [8]. The angiography is diagnostic and therapeutic procedure which guides embolization, when fertility is required. Others therapeutic procedures such as the resection of the fistula or the hysterectomy can be performed. [14].
These cases report highlights our experience with two patients having this rare morbidity and treated differently. The embolization of UAVM reveals effective for the management of this kind of vascular malformation.
Case reports
Case 1
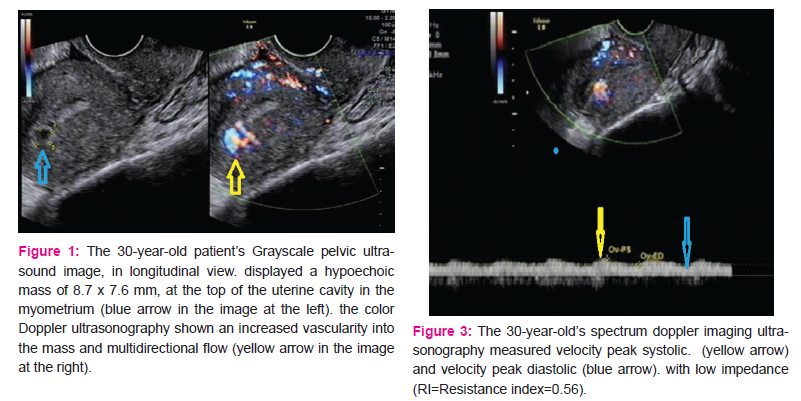
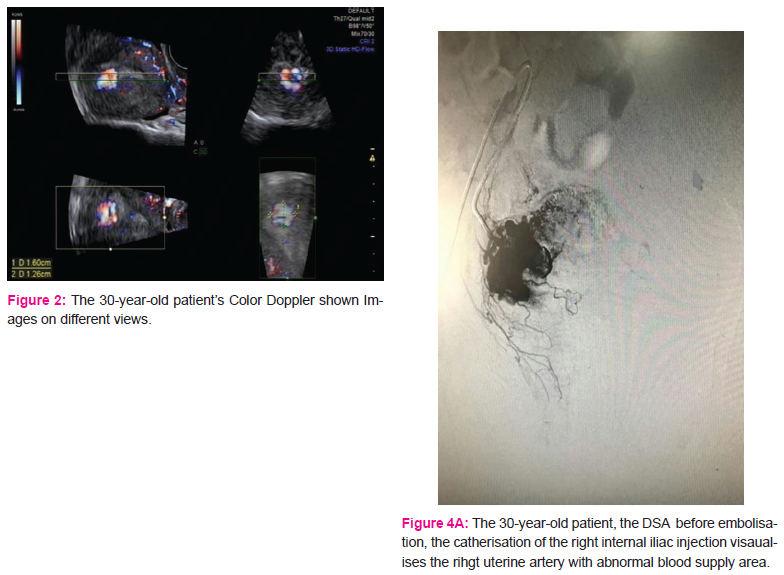
A 30- year-old patient gravida 1 para 1 complained of slight vaginal bleeding and fever, 15 days following a cesarean section delivery of a baby weighing 3900g. She has no history of coagulation disorder. She had normal vital signs, fever 38.4oC, the uterus was slightly tonic, the pelvic ultrasound was normal. Accordingly, she was treated by anti-inflammatory, antibiotics and oxytocin. She was discharged after 3days with complete resolution of symptoms. On postpartum day 31, she was readmitted in the emergency ward for heavy vaginal bleeding (the hemoglobin level 87g/l,CRP: 28.73mg). She was transfused with 1 unit of red blood cells and treated with oxytocin and antibiotics for Escherichia coli vaginitis. The pelvic color Doppler ultrasound shown a tortuous mass in the myometrium with no significant blood flow signal (figures 1, 2). She had intermittent bleeding on the second day of hospitalization (the hemoglobin level 74g/l). Consequently; she was transfused with 2 units of red blood cell. The subsequent color and spectral Doppler ultrasound revealed a sign of blood flow with low impedance and high velocity in the myometrium of the uterus body (Figure 3). The diagnosis of an arteriovenous malformation was considered; in order to confirm and assess the extent of the lesion, further MRI was done. She was referred to the interventional radiology where a DSA was done; displaying a right uterine arteriovenous malformation (Figure 4. A). Then, the right uterine artery embolization was performed (Figure 4. B). The patient was discharged home without any symptoms. The menstrual cycle became normal, and she did not have any recurrence within 3 years of follow up.
Case 2
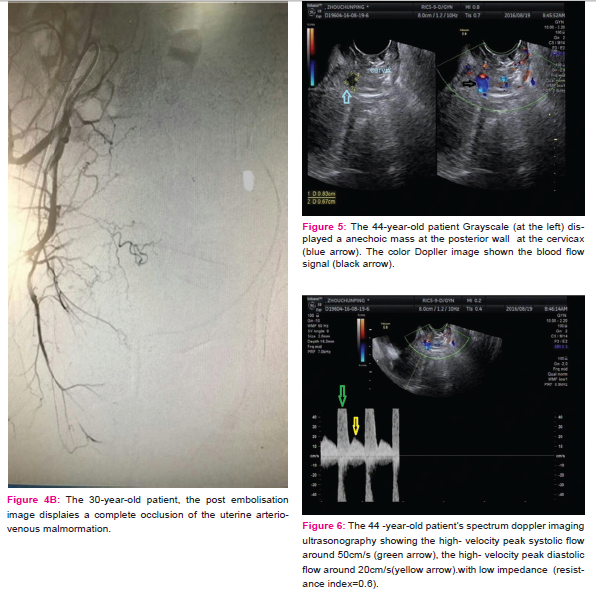
A 44 -year-old patient gravida 2, para 1, Abortion 1 was admitted for vaginal bleeding. She had a history of curettage for termination of a pregnancy and a history of cervical conization (for a CINIII with HPV 16 positive) one week earlier. She was clinically instable, Hemoglobin concentration: 79g / L, she was transfused with 2 units of red blood cells; therefore, the CDFI revealed a heterogeneous tubular hypoechoic structure, hypervascularized with a peak systolic and diastolic velocity, on the posterior wall of the cervix (Figures 5 and 6). On day 13, she presented a heavy vaginal bleeding, on the subsequent ultrasound, the findings were similar to the previous examination, and consequently she obtained the diagnosis of a uterine arteriovenous malformation. A Transvaginal bilateral uterine artery ligation has been done. The post operatory period was uneventful and she was discharged home. 1 week later, she presented with another bleeding; after counseling, she underwent a transabdominal total hysterectomy and bilateral salpingectomy. In vitro specimen from the cervix reported an arteriovenous fistula at the right posterior wall of the cervical canal. She had no further hemorrhage during a follow up of 6 months.
Discussion
The UAVM is an abnormal connection between an artery and a vein circumventing the capillary system [8,10,12,14]. There are two categories. The congenital subset is due to a disturbance during embryogenesis, concerning vessel differentiation, and induces many vascular connections[3,5, 7].While, the acquired one represents a sole joining between an artery and a vein [ 5, 10]. The acquired subtype, also known as “fistulae” [5, 8] is a consequence of mechanical trauma, such as normal delivery, cesarean [5,6, 11,], inflammation, neoplasm, intrauterine surgical procedures like the dilatation–curettage [6, 10, 12, 15] and the hysteroscopy. Others risk factors include hysterectomy, gestational trophoblastic disease and maternal exposure to diethylstilbestrol [4, 15].
The UAVM can lead to a torrential and recurrent gynecological bleeding [2, 10]; previously, the diagnosis was made by the histopathology of a uterine specimen. Currently, the ultrasonography and MRI are the non-invasive tools used. The grayscale ultrasound shows an anechoic, tubular or sinusoidal structure in the myometrium [5]. In addition, the color Doppler ultrasound visualizes the tortuous blood flow, while the Spectral Doppler further displays the peak speed of blood wave [5]. Thus, expresses low impedance by resistance index calculation [7, 13, 16]. Therefore, the spectral Doppler differentiates the UAVM to others hypoechoic images seen in grayscale US such as retained product of conception. MRI, CT and CT Angiography are used for large UAVM [7,12].
The Angiography is the cornerstone of the diagnosis [7]. The embolotherathy is widely used with success and fertility is therefore preserved [7,12]. However, hysterectomy is the definitive treatment, frequently when the conservative treatment fails.
A systematic review of Panagiotis Peitsidis et al., assessed 103 patients; all of them underwent Doppler US and Angiography for diagnosis. 62 out of 103 patients underwent embolization with a failure rate of 12, 6% [7].
Among the included patients, we reported a case of arteriovenous fistula following a cervical conization (case 2). This case is of interest; since a fistula following a conization is unusual, with many risk factors such as CINIII and previous curettage. A hysterectomy was done after a transvaginal bilateral uterine artery ligation has failed. Another patient (case 1) had a fever after cesarean that may precipitate the formation of the fistula, she has been treated with embolization
using gelatin sponge (Gelfoam) with good outcome. Others embolization agents have been reported in the literature, Tris-Acryl-gelatin and Polyvinyl alcohol particles being examples [7]. In fact, our 2 patients were at high risk because of the combination of risk factors, according to the pathophysiology reported in a systematic review of Daniel et al [11].
The treatment of UAVM is not standardized; However, depends on the clinical condition of the patient, desire of fertility and age [13]. Before performing curettage for unknown vaginal bleeding, a better assessment of the cause is required to prevent profuse hemorrhage [16]. Because of ionization side effects[10], Because of ionizing effects, angiography diagnosis should only be completed to guide embolization [14].
Our limitation is based on the fact that the diagnosis was not made promptly, while our strength is the length of follow up.
Conclusion: Uterine arteriovenous malformation is a rare and life-threatening condition. Clinicians should always consider a UAVM in a case of periodical bleeding after a uterine trauma, such as a curettage [5]. The Spectral flow and Doppler ultrasonography helps the diagnosis, but requires adequate skills [7]. The embolotherapy is affective; however, the hysterectomy remains the last management for difficult and dangerous UAVM.
List of abbreviations
UAVM: Uterine arteriovenous malformation
CDFI: Color Dopplerflowwith spectral imaging
DSA: Digital subtraction imaging
CT: Computed tomography
MRI: Magnetic resonance imaging
CIN: Cervical intraepithelial neoplasia
CRP: C- reactive protein
HPV: Human papilloma virus
Acknowledgements
The authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors /
publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
The authors are also thankful to the ultrasound department of Dalian Gynecology and Obstetrics (Maternal and child health care) Hospital affiliated to Dalian Medical University and to the Interventional radiology department of Dalian central hospital for their collaboration.
References:
1. Farias M, Santi C, Lima A, Teixeira S, De Biase T. Radiological findings of uterine arteriovenous malformation: a case report of an unusual and life-threatening cause of abnormal vaginal bleeding. Radiol Bras. 2014 Mar/Abr;47(2):122–124.
2. Kylie Hae-Jin Chang., et al., Uterine arteriovenous malformation caused by intrauterine instrumentation for laparoscopic surgery due to left tubal pregnancy. ObstetGynecol Sci. 2014; 57(5):419-423.
3. Jacques L, Lund M and Baruah D. Uterine Arteriovenous Malformations: A Rare Cause of Vaginal Hemorrhage after Hysterectomy. 2016; Vol.2 No.2:29.
4. Taehwan K, Ji H, JinooK, Hyun-Ki Y,Gi-Young K, Dong-Il G,et al. Management of Bleeding Uterine Arteriovenous Malformation with Bilateral Uterine Artery Embolization, Yonsei Med. 2014; 55: 2.
5. Natali A, Tiffanee A, Brook J, Deirdre J.. Postpartum Uterine Arteriovenous Fistula, Obstet Gynecol. 2004;103:1076–8.
6.Yasmine A, Jon D, Nami A. Ultrasound-guided Transcutaneous Embolization of Uterine Arteriovenous Fistula Performed for Treatment of Symptomatic, Heavy Vaginal Bleeding: Case Report with Brief Review of Literature, Journal of Medical Ultrasound. 2015; 23: 146-149.
7. Panagiotis P, Emmanouil M, Vasiliki T, Rolf K ,Lukas S. Uterine arteriovenous malformations induced after diagnosticcurettage: a systematic review, Arch Gynecol Obstet. 2011; 284:1137–1151.
8. Lisa H, Tracy C. Marchant, D, Douglas C. and Amanda J. Scherbel, BS. Vascular Malformations: Classification and Terminology the Radiologist Needs to Know, Semin Roentgenol 2012;47(2):106–117.
.9. Mulliken JB, Glowacki J: Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg. 1982; 69:412-422.
10.Ravi Srinivasa,et al., Transcatheter Percutaneous Embolotherapy of Uterine Arteriovenous Malformations: A Report of 2 Cases, J Women’s Health Care 2015; 4:4.
11. Daniel J, Megan J, Jamal A, Catalin B, Joshua D.A Systematic Review of Acquired Uterine Arteriovenous Malformations: Pathophysiology, Diagnosis, and Transcatheter Treatment, Am J Perinatol Rep. 2016;6:6–14.
12. Geetha Visvalingam, et al., An Unusual Case of Acquired Uterine Arteriovenous Malformation with Persistent Scar Ectopic Pregnancy Successfully Managed with Uterine Artery Embolization, JJ Med Cases. 2016;7(4):143-147.
13. Hilwati H, Ouzreiah N. Uterine Arteriovenous Malformation, Malays J Med Sci. 2013; 20(2): 76-80.
14. Andrew M, Montu P, Navid E , Mandy W, Cynthia H, Harold N. Diagnosis and Treatment of an Acquired Uterine Arteriovenous Malformation in a 26-Year-Old Woman presenting with Vaginal Bleeding.2015, 167: 198-22115.
15.Tom M, Victor H, , and Eric G. Uterine Arteriovenous Malformation - A Rare Cause of Uterine Haemorrhage, Aust NZ J ObstetGynaecol1994; 34 2 197.
16.D. Timmerman, J. Wauters, S. Van, D. Van , G. Maleux, T. Van et al. Color Doppler imaging is a valuable tool for the diagnosis and management of uterine vascular malformations, Ultrasound Obstet Gynecol. 2003; 21:570 – 577.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License