IJCRR - Vol 09 issue 10 current issue , May, 2017
Pages: 19-22
Date of Publication: 27-May-2017
Print Article
Download XML Download PDF
Epidemiology of Animal Bites with Special Reference to Post-exposure Prophylaxis of Rabies in and Around Malda, West Bengal: A Hospital-based Study
Author: Arindam Karmakar, Aishwarya Bhattacharya
Category: General Sciences
Abstract:Background: Bites from stray dogs are the reason of rabies infection in India most of the time, whereas bite of several other animals such as cats, monkeys, jackals and wolves may cause rabies. People of poor socio-economic class are the majority of victims. Lack of knowledge regarding primary wound management and requirement of post-exposure prophylaxis prevails in a large part of our country.
Objectives:
1. To assess the epidemiological profile of animal bite victims.
2. To assess the adherence to the present post \? exposure prophylaxis protocol.
3. To assess the present practice and knowledge regarding treatment of animal bites.
Materials and Methods: Total 100 animal bite victims attending the Rabies vaccination clinic at Malda Medical College and Hospital, Malda, West Bengal were interviewed using a pre-tested questionnaire format.
Results: Majority of the victims were from lower income group (58%). 62% were male. The biting animal was mostly dog (82%). 69% patients were bitten on lower extremities; 61% having grade III exposure, the rest being grade II exposures.
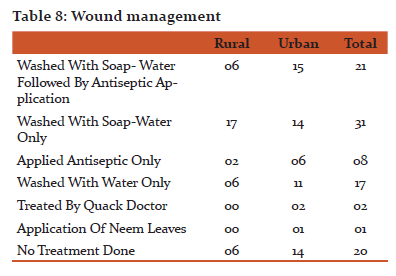
Only 21% of the victims took proper care of the wound; whereas, a considerable number (20%) took no care of the wound at all.
All the patients were administered anti-rabies vaccine but only one patient with grade III exposure was administered rabies immunoglobulin. The victims showed inadequate knowledge regarding primary wound management.
Conclusion: Lack of awareness and motivation were significant reasons for poor wound-care and failure to adhere to the post-exposure prophylaxis schedule apart from great distance from the vaccination clinic and unavailability of rabies immunoglobulin
Keywords: Animal bite, Malda, Post-exposure prophylaxis, Rabies
Full Text:
INTRODUCTION
Rabies has been endemic in India since time immemorial and about 20,000 persons die of rabies each year.1 Most of these victims (97%) are attributed to bites by dogs which is the major reservoir of this disease. Bites by several other animal species like cats, monkeys, jackals and wolves may cause rabies. A WHO-sponsored multi-centric study conducted all over India in 2003 revealed that people of poor socio-economic class both in rural and urban populations were the majority of animal bite cases. Dogs, mainly stray dogs were the major culprits. A considerable proportion of the persons did not take initial care of the wound; many of them did not opt for Anti-Rabies vaccine and too few persons were administered Rabies- Immunoglobulin.2 But in a country as diverse as ours, the importance of local data regarding the profile of animal bite victims, status of post-exposure prophylaxis of rabies and the status of knowledge and practice of common people cannot be overemphasized. This study was designed to assess the epidemiological profile of the animal bite cases coming to the Emergency and Outpatient department of Malda Medical College & Hospital, Malda. Information was gathered to assess the knowledge and practice of animal bite victims regarding immediate management and post-exposure prophylaxis of rabies.
OBJECTIVES
- To assess the epidemiological profile of animal bite victims.
- To assess the adherence to the present post – exposure prophylaxis protocol.
- To assess the present practice and knowledge regarding treatment of animal bites.
METHODOLOGY
The cross-sectional study was done at the Rabies vaccination clinic of Malda Medical College & Hospital, Malda. Animal bite victims were enquired using a pre-tested questionnaire format (annexure 1) after receiving informed consent from the patients. Convenient sampling during the month of May, 2014 was done.
RESULTS
Total 100 patients were interviewed. After the analysis of the collected data it was found that 37 persons were from rural areas whereas 63 patients were from urban areas. Males (62%) were more affected than females (38%). (Table 1)
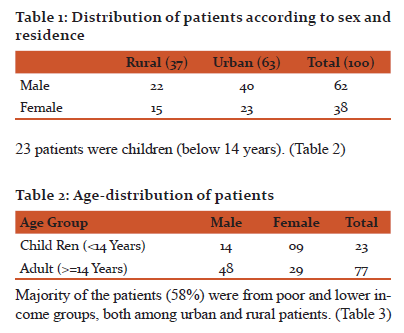
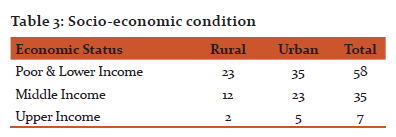
Majority of the patients (58%) were from poor and lower income groups, both among urban and rural patients. (Table 3)
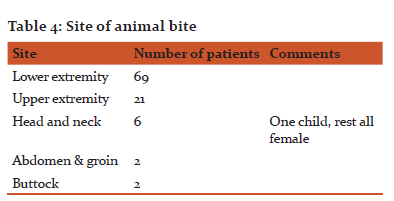
The site of bite was lower extremities in most of the cases (69%) followed by upper extremity (21%), head and neck (6%), buttocks (2%) and abdomen and groin (2%). Interestingly all the persons bitten in the head & neck were female including one girl child. (Table 4)
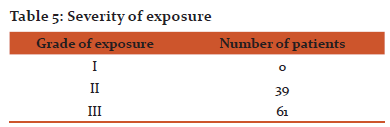
Majority of the patients suffered from grade III exposure (61%). Rest had grade II exposure. As it was a vaccination clinic based study, no persons having grade I exposure turned up as there is no need of vaccination in grade I exposure. (Table 5)
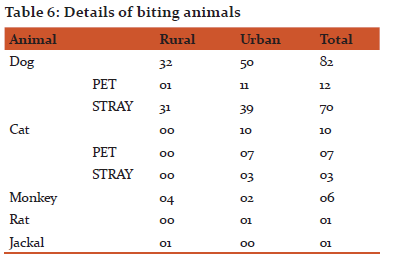
The biting animal was in most of the cases dogs (82%) followed by cats (10%) and monkey (6%). Single cases of rat bite and jackal bite were also present. Most of the dogs were stray whereas most of the cats were pets. (Table 6)
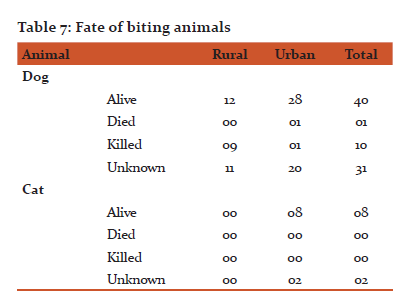
Out of the 82 dog bite cases, 40 dogs were alive, 01 died during the observation period of 10 days and 10 dogs were killed by people. The status of the rest 31 dogs was unknown. It is evident from the Table 7 that dogs were killed mostly in the rural areas. Most cats were alive.
Regarding the wound care (Table 8), 21 patients washed the wound with soap-water and applied antiseptic on the wound, 31 patients washed with soap-water only and 08 persons applied antiseptic only. Rest of the patients resorted to washing with water (17), being treated by quack doctors (02), application of neem leaves (01) and taking no care of the wound at all (20).
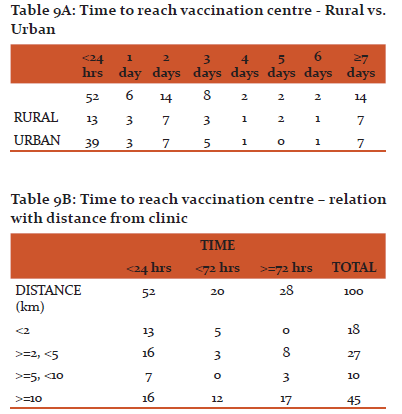
All the persons coming to the clinic received anti rabies vaccines. However, only one person received anti-rabies immunoglobulin. On examination of the time taken to reach the vaccination centre after the exposure in terms of rural and urban population as well as relation with the distance from the vaccination centre (Table 9A and Table 9B) it is apparent that
- A considerable proportion of the patients failed to turn up at the clinic within 24 hours
- Even a delay of more than 7 days was quite common (14%)
- Both the rural as well as urban populations show similar trends.
- The number of people coming very late to the clinic (more than 72 hours) increased with increasing distance from the clinic but a considerable number of patients living within 10 kms (11% patients) came very late.
- A significant proportion of patients living more than 10 kms far from the vaccination center turned up within 24 hours.
Average distance from vaccination clinic was 10.5 kms
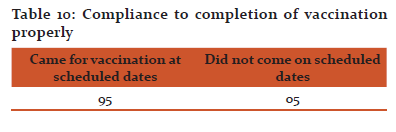
While the patients were enquired regarding the adherence to the vaccination schedule only 5% of the patients (5 patients) were found to have missed the prescribed date for vaccination. On a closer look at the persons with poor compliance it was found that 2 of them lived at a distance of more than 50 kms from the clinic. The other 3 patients were from urban population and lived at a distance of 10 kms or less from the clinic and all of them class II exposure. (Table 10)
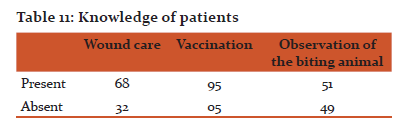
Upon questioning regarding the knowledge of the patients regarding wound care, importance of anti-rabies vaccination and the importance of observation of the biting animal, it was discovered that 68% of the victims had the knowledge of primary wound care; 95% had the knowledge of the importance of anti-rabies vaccination and 51% had the knowledge of importance of observing the biting animal for 10 days. (Table11)
DISCUSSION
This was a vaccination-clinic based study with the hospital situated at Malda town, the district headquarter of Malda district. So evidently the most of the bite victims (63%) were from urban Population. Majority were from lower income group in both urban and rural groups. Males (62% including male children) and children (23%) were frequently affected probably due to outdoor activities of males and the mischievousness and carelessness of the children. This finding is similar to other studies held across India 2, 3, 4, 5 as well as around the world 6, 7. In agreement with other studies, the biting animal was dog in most of the cases (82%) followed by cats (10%) and other animals. Most of the dogs were stray. 2, 3, 5 Like in other studies, extremities were the most frequent site of bite. 1, 3, 7
The primary management of the wound at the bite site was not satisfactory similar to other studies in India. 2, 3, 8
As this was a vaccination clinic based study all the patients had been receiving vaccination contrary to the community based studies performed elsewhere in India.
However, only one patient out of the 61 category III bites received Rabies immunoglobulin which reflects the tendency in other parts of the country. 1, 3, 9 Unavailability of rabies immunoglobulin was the reason of the failure to administer RIG in this study. Only one patient could be convinced to purchase the expensive immunoglobulin from market.
Just as the study conducted by Ichhpujani RL et al 8, knowledge on wound care after animal bite was inadequate amongst the victims.
CONCLUSION
This vaccination-clinic based study at Malda points out the fact that the cause of delay, failure or poor adherence of the animal bite victims to medical care is on many occasions, a lack of knowledge and motivation, apart from distance from the clinic and loss of working hours. It emphasizes the importance of information, education and communication activities regarding animal bites to motivate the victims to seek appropriate medical attention in time. Widespread availability of treatment of animal bite cases with constant supply of vaccine and immunoglobulin is also essential if elimination of rabies has to be achieved in near future.
Conflict of interest: nil
Source of funding: nil
Acknowledgement: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Sudarshan M, Madhusudana S, Mahendra B, Rao N, Ashwath Narayana D, Abdul Rahman S, et al. Assessing Burden of Rabies in India. Report of a WHO Sponsored National Multi-Centric Rabies Survey. International Journal of Infectious Diseases 2007;11:29-35.
2. Sudarshan M, Mahendra B, Madhusudana S, Ashwath Narayana D, Rahman A, Rao S, et al. An Epidemiological Study of Animal Bites in India: Results of a WHO Sponsored National Multi-Centric Rabies Survey. J. Commun. Dis. 2006;38(1):32-39.
3. Ichhpujani R, Mala C, Veena M, Singh J, Bhardwaj M, Bhattacharya D, et al. Epidemiology of animal bites and rabies cases in India. A multicentric study. The Journal of Communicable Diseases 2008 March;40(1):27-36.
4. Agarwal N, Reddajah V. Epidemiology of dog bites: a community-based study in India. Tropical Doctor 2004;34(2):76-78.
5. Shetty R, Chaturvedi S, Singh Z. Profile of animal bite cases in Pune. The Journal of Communicable Diseases 2005 March;37(1):66-72.
6. Eng T, Fishbein D, Talamante H, Hall D, Chavez G, Dobbins Jea. Urban epizootic of rabies in Mexico:epidemiology and impact of animal bite injuries. Bulletin of the World Health Organization 1993;71(5):615-24.
7. Cleaveland S, Fe`vre EM, Kaare M, Coleman PG. Estimating human rabies mortality in the United Republic of Tanzania from dog bite injuries. Bulletin of the World Health Organization 2002;80(4):304-10.
8. Ichhpujani R, Chhabra M, Mittal V, Bhattacharya D, Singh J, Lal S. Knowledge, attitude and practices about animal bites and rabies in general community--a multi-centric study. The Journal of Communicable Diseases 2006 December;38(4):355-61.
9. Mondal T, Ray Karmakar P. Care of animal bite victim in Community and in health care facility in a rural area of West Bengal. IOSR Journal of Dental and Medical Sciences 2016 Jan;15(1, version IV):01-04.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License