IJCRR - 5(17), September, 2013
Pages: 95-101
Date of Publication: 12-Sep-2013
Print Article
Download XML Download PDF
A STUDY OF COMPLICATIONS OF THYROIDECTOMY
Author: Sudarshan Babu K. G., Lakshmi Shantharam
Category: Healthcare
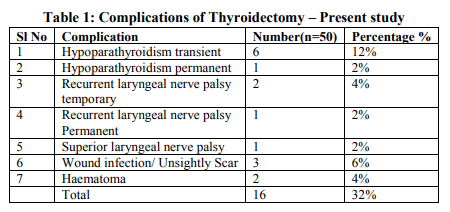
Abstract:Introduction: Thyroid surgeries are the most common endocrine surgeries performed today. This procedure has been through tremendous evolution to make it a safe procedure. In spite of improved techniques, every thyroid surgeon has come across complications associated with this surgery. This study aims to understand various complications after thyroid surgeries and the factors responsible for complications and discuss management techniques for those complications in brief. Materials and Methods: 50 patients admitted in our hospital for various thyroid surgeries were followed up from pre operative evaluation to post operative period for appearance of complications. Those with postoperative complications were followed up and managed. Results: 12% patients had transient hypoparathyroidism, 2% had permanent hypoparathyroidism, 4% had temporary RLN palsy and 2% had permanent RLN Palsy. Other rare complications were Superior laryngeal nerve palsy, hematoma, and wound infection. Conclusion: In our study, temporary hypoparathyroidism was the most common complication (12% of the patients operated). Improved surgical techniques during thyroid surgery and efficient methods of complication management have reduced the postoperative morbidity and mortality. In spite of all measures, keen observation in postoperative period is important to look for complications for early intervention.
Keywords: Thyroidectomy, Recurrent Laryngeal Nerve palsy, Hypocalcemia, Complications
Full Text:
INTRODUCTION
Thyroid surgery is one of the common endocrine surgeries performed today. Thyroid gland is situated in a critical area in the neck surrounded by many vital structures. The complications related to the surgery were very high in olden days. This surgery did not find ready acceptance by Germans and French initially who called these operations “Foolhardy Performances”. 1 Any discussion on thyroid surgeries will be incomplete without the mention of “Theoder Kocher” a magnificent surgeon who reduced the mortality of thyroid surgeries from 50% to less than 4.5% by advocating methodical surgical dissection of the gland.2 Kocher received Nobel prize in the year 1909 for his pioneer work.1 Despite continuous efforts by surgeons all over the world for making this essential surgery free of morbidity, it continues to be an enigma and some kind of complication has become a rule rather than an exception. This study aims to identify various complications arising in thyroid surgery and literature review for factors predisposing for complications and methods of preventing and managing those complications.
MATERIALS AND METHODS
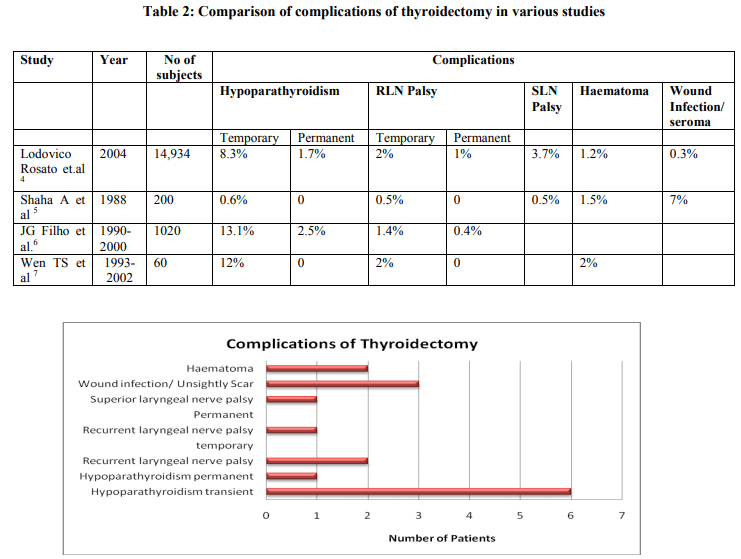
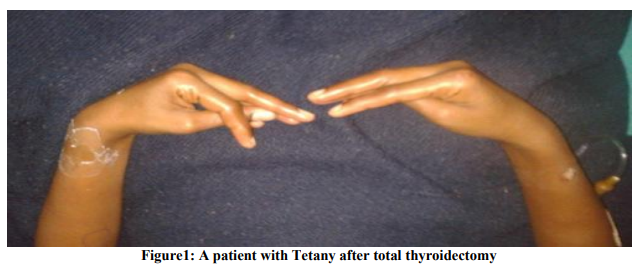
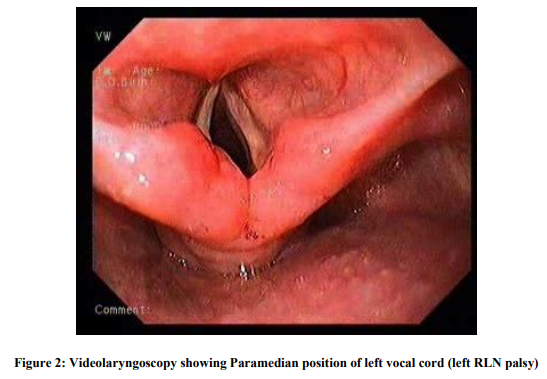
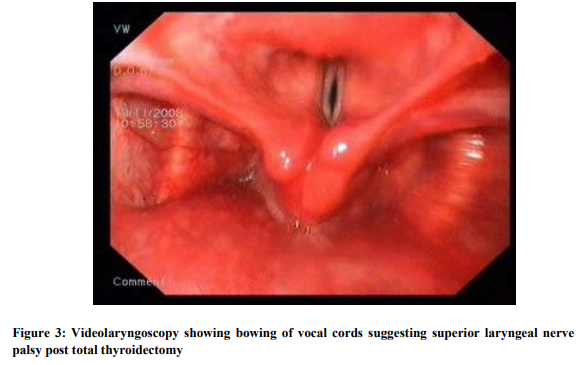
The present study was conducted at Kempegowda Institute of Medical Sciences, Bangalore and includes 50 patients admitted in the department of surgery wards for various thyroidectomy procedures. The patients requiring thyroid surgery and those willing to undergo surgery and attend follow up were included in the study. It was a prospective observational study. Informed written consent was obtained from all patients, which was approved by the institutional ethics committee. Patients who had complications prior to surgery and those who were lost for follow up were not included in the study. A detailed history was taken and thorough clinical examination was done. Vocal cords assessment was done preoperatively using Videolaryngoscopy and documentation done. Pre operatively the thyroid profile, ultrasound of thyroid and fine needle aspiration cytology of the thyroid nodule was done along with routine urine and haematological examinations. Depending on the need of the clinical condition the thyroid surgery was planned. The procedures were done under general anaesthesia. All the operations of the present study were done by the same team of surgeons headed by the most senior surgeon of the unit to exclude surgeon related and experience related variables. During surgery effort was made to identify and preserve all the Parathyroid glands. When excision was inevitable, it was planted in the sternocleidomastoid muscle. The recurrent laryngeal nerves were not dissected for identification in all cases. Soon after the procedure at the time of extubation, the anaesthesiologists using the videolaryngoscopy demonstrated the mobility of the vocal cords. Patients were followed up for 2 months. If any complication was noticed, that patient was followed up for 1 year. RESULTS 50 patients undergoing various thyroid surgeries were included in the study. Out of them 42 were females and 8 were males constituting 84% and 16% respectively. Majority of the patients were in 4th decade with 19 patients constituting 38%. Benign solitary nodule was the commonest condition in our patients study with 23 patients (46%) in that category. Most common malignant condition detected was papillary carcinoma of thyroid. Surgical procedures performed were hemithyroidectomy, subtotal thyroidectomy, isthmusectomy and total thyroidectomy. Hemithyroidectomy was the commonest procedure done. The same team of surgeons performed all procedures in order to avoid the surgeon related variability. Complications of surgery were looked for during the postoperative visits till 2 months after surgery in all patients. 16 out of 50 patients had one or more complications that amounted to 32%. Those with complications were followed up for 1 year. The commonest complication in our study was hypoparathyroidism. (Table 1) Out of total 50 patients 7 showed features of hypoparathyroidism amounting to total 14% among which 6 had transient hypoparathyroidism(12%) and 1(2%) had permanent hypoparathyroidism. Patient complaints included perioral numbness, tetany of hands (Fig 1) and spasm of calf muscles. They were treated with intravenous Calcium Gluconate injection followed by oral calcium with vit D3 supplements three times a day for 10 days. One patient had symptoms in spite of many days of calcium supplement who was asked to take daily calcium supplement. Recurrent laryngeal nerve (RLN) palsy was noted in 3 patients. 2 had unilateral and 1 patient had bilateral palsy. (Fig 2) Both the patients with unilateral RLN Palsy recovered by 6 months. All the patients with recurrent laryngeal nerve palsy were treated with Inj dexamethasone 8 mg three times a day and speech therapy for vocal cord exercises. One patient had bilateral abductor palsy. He was a patient of thyroiditis with extensive fibrosis and neovascularization. Vocal cords were immobile at the time of extubation and patient developed stridor. Tracheostomy was done. Patient was followed up regularly for recovery of vocal fold movements. After 1 year when there were no signs of recovery of vocal cords, Laser arytenoidectomy was done and patient was decannulated from the tracheostomy tube. Haematoma was seen in 2 (4%) patients. In one patient who underwent isthmusectomy, the drain was not kept as there was a good operative field with very minimal bleeding. Thyroid bandage was applied to approximate the flaps. The haematoma noticed on 1st postoperative day was cleared by wide bore needle aspiration and releasing one suture. One patient (2%) had superior laryngeal nerve palsy and he presented with vocal fatigue and frequent throat clearing. On Videolaryngoscopy, bowing of vocal cords noted. (Fig 3) Patient was treated with steroid injections and vocal exercises were taught. After 15 days, patient showed recovery of vocal cords. 3 patients (6%) had wound infection, which was treated with appropriate antibiotics and regular dressing. One patient developed hypertrophic scar that was treated with intralesional Triamcinolone injection and scar thinning was achieved partially.
DISCUSSION
Thyroid surgery is the most common endocrine surgery performed. Most of the multinodular goiters require excision of both the lobes of thyroid with the isthmus. Subtotal thyroidectomy was a standard practice, but recurrence rate with this procedure is as high as 10-30%. 3 Total thyroidectomy is free of this problem but poses potential high risk of complications. Major complications of thyroidectomy are Hypocalcaemia, Recurrent Laryngeal nerve (RLN) Palsy and postoperative bleeding. Less common complications are surgical site infections stitch sinus, granuloma, keloid formation, wound infection and chylous fistula.2 The prevalence of complications varies from 5-27.5% in various studies. 1 Transient Hypoparathyroidism is the most common complication. (Table 2) 4,5,6,7 Factors responsible for complications: 8,9,1 ? Extended thyroidectomy (total thyroidectomy) ? Revision surgery ? Patients older than 50 years ? Graves disease ? Surgeon`s experience ? Dissection extended to identify the recurrent laryngeal nerve ? Central node neck dissection ? Extended Operating time10 ? Weight of the gland10 ? Substernal goiter with tracheal compression 7 Special surgical training and expertise is required while operating on high-risk conditions like total thyroidectomy and graves disease. The risk of hypocalcemia after thyroid surgery varied in different studies with a range of 2.43% to 35.49%.1 At least two parathyroid glands should be identified and preserved.9 Postoperative Hypoparathyroidism commonly occurs due to removal or devascularization of the parathyroid glands. Parathyroid autotransplantation helps to restore the parathyroid function and avoids the need for prolonged pharmacological support. Overall success rate with the immediate parathyroid autotransplantation into the sternocleidomastoid muscle ranges from 85- 95%.11 Routine supplementation with Oral calcium and vitamin D prevents symptomatic postoperative hypocalcemia without inhibiting the parathormone secretion and thereby facilitating short hospital stay.12 Postoperative vocal cord palsy is defined as the presence of an immobile vocal cord or the decreased movement of the vocal cord during phonation. Postoperative RLN palsy has the potential for recovery with a rate ranging from 50- 88%. The RLN palsy is regarded as permanent if it persists for more than 1 year after the surgery. 10The risk of permanent vocal cord paralysis varies from 0.2-5% in literature.1 Various mechanisms have been suggested for vocal cord palsy associated with thyroidectomy. Compression of the RLN and its blood supply, stretching of the nerve, inflammation or edema of RLN as in thyroiditis are suggested to be the aetiological factors.13 Vocal cord examination is mandatory pre-operatively and postoperatively during extubation. There are different schools of thought for the visualization of recurrent laryngeal nerve during surgery. Some surgeons advocate that intraoperative verification of anatomical and functional integrity of the RLN is important to avoid potential nerve injury and vocal cord palsy. 14 Wade advocated that the RLN is very vulnerable and the nerve should not be visualized or touched.15 Intraoperative nerve monitoring device helps to monitor RLN during surgery by providing both auditory and visual evoked waveform information.14 However the nonrecurrent laryngeal nerve on the right side is always a threat to indirect injury because of its rare occurrence.10 For those nerves cut unintentionally, recognized intraoperatively, endto-end anastomoses of the nerve or Ansa-RLN anastomoses may be tried. Teflon injection and Isshiki type I Thyroplasty are other treatment methods.16 Postoperative hematoma is another complication that can be fatal. Close postoperative monitoring of patient for hematoma is essential. Early exploration and evacuation of hematoma in all patients who develop postoperative hematoma is important, however a conservative approach may be tried in minimal hematoma without progression.17 A Precise tracking of the complications in a thyroid surgery helps surgeon in taking quick remediable action. This analysis helps patients to get correct information prior to surgery to make a conscious and informed decision about the surgery. When residents under training perform thyroidectomy, it can be made safe when done under close supervision of experienced faculty.18
CONCLUSION
Temporary hypoparathyroidism is the most common complication in the literature including our study. R L N Palsy and Haematoma are other dreaded complications. It has been a century since the great surgeon “Theodore Kocher” received Noble prize for his contribution in taking this surgery to a new safe level, but still this procedure continues to pose challenges for the most experienced surgeons also. It is essential to keep in mind the possible complications in this procedure and be prepared to mange them. Good surgical expertise is essential to avoid complications. Keen postoperative monitoring of patient is invaluable and helps in early detection and management of those complications.
References:
1. Sumit Gupta, C Vasu Reddy, Shyam TC, Smriti Karki. Clinicopathological features and complications of thyroid operations: A Single centre experience. Indian J Otolaryngol Head Neck Surg (April-June) 2013; 65(2):140-145.
2. Tariq wahab khanzada, Abdul Samad, Waseem Memon, Basanth Kumar. Postthyroidectomy complications: The Hyderabad experience. J Ayub Med Coll Abbottabad 2010; 22(1): 65-68.
3. Antorio RZ, Jose Rodriguez, Jaun Riquelme, Teresa Soria, Manuel Canteras, Pascual Parrilla. Prospective study of Postoperative complications after Total Thyroidectomy for Multinodular goityers by surgeons with experience in Endocrine surgery. Ann Surg. 2004 July; 240(1): 18-25.
4. Lodovico Rosato, Nicola Avenia, Paolo Bernante, M Aurizio De Palma, Giuseppe Gulino, Pier Giorgio Nasi et al. Complications of Thyroid surgery: Analysis of a multicentric study on 14,934 patients operated on in Italy over 5 yrs. World Journal of Surgery; March 2004; Vol 2893): 271-276.
5. Shaha A, Jaffe BM. Complications of thyroid surgery performed by residents. Surgery. 1988 Dec; 104(6): 1109-14.
6. JG Fillo, LP Kowalski. Surgical Complications after thyroid surgery performed in a cancer hospital. Otolaryngology- Head and Neck Surgery. Mar 2005; Vol 132(3): 490-494.
7. Wen TS, Electron Kebebew, Quan-yang Duh, Orlo HC. Predictors of Airway Complications After Thyroidectomy for Substernal Goiter. Arch Surg.2004; 139(6): 656-660.
8. Y Erbil, U Barbaros, H Issever, I Borucu, A Salmaslioglu, O Mete et.al. Predictive factors for recurrent laryngeal N plasy and hypoparathyroidism after thyroid surgery. Clinical otolaryngology; Feb 2007; Vol 32(1): 32-37.
9. Oliver Thomusch, adreas machens, Carsten Sekulla, Michael Brauckhoff, Henning Dralle. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: A multivariate analysis of 5846 consecutive patients. Surgery; Feb 2003; Vol 133(2): 180-185.
10. Chung-Yau Lo, Ka-Fai Kwok, Po-Wing Yuen. A Prospective Evaluation of Recurrent Laryngeal Nerve Paralysis during Thyroidectomy. Arch Surg. 2000; 135(2): 204-207.
11. Christakis I, Constantinides VA, Tolley NS, Palazzo FF. Parathyroid Autotransplantation during Thyroid Surgery. World J Endocr Surg, Sept-Dec 2012;4(3):115-117.
12. Bellantone R, Lombardi CP, Raffaelli M, Boscherini M, Alesina PF, De Crea C et al. Is Routine supplementation therapy (Calcium with Vitamin D) useful after Total thyroidectomy? Surgery. 2002 Dec; 132(6): 1109-12.
13. Deependra NS, Amit Agarwal, Sushil Gupta, Manoj Jain. Benign thyroid Disease causing RLN Palsy. World J Endocr Surg, May-Aug 2011; 3(2):65-68.
14. Poveda MCD, Dionigi G, Sitgesserra A, Barczynski M, Angelos P, Dralle H etal. Intraoperative Monitoring of the Recurrent Laryngeal Nerve during Thyroidectomy: A Standardized Approach part 2. World J Endocr Surg 2012; 4(1): 33-40.
15. JSH Wade. Vulnerability of the recurrent laryngeal nerves at thyroidectomy. Br j Surg, 43(1955), pp 164-179.
16. Feng-Yu Chiang, ling-Feng wang, Yin-Feng Huang, ka-Wo Lee, Wen-Rei Ko.Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery. Mar 2005; Vol.137 (3): 342- 347.
17. Ashok RS, Bernard MJ. Practical management of post thyroidectomy hematoma. Journal of Surgical Oncology. Dec 1994; Vol 57(4): 235- 238.
18. Maisie LS, Uttam KS, Dale H Rice. Safety of thyroidectomy in residency: A review of 186 consecutive cases; Nov 1995; Vol 105(11): 1173-117
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License