IJCRR - 5(18), September, 2013
Pages: 54-59
Date of Publication: 25-Sep-2013
Print Article
Download XML Download PDF
EVALUATION OF AGE RELATED MACULAR DEGENERATION AMONG PATIENTS WITH CHRONIC OBSTRUCTIVE PULMONARY DISEASE IN A TERTIARY HEALTH CARE CENTRE
Author: Somanath Dash, Satish K., Mishra S. K. , P.Harshavardhan V.
Category: Healthcare
Abstract:Chronic obstructive pulmonary disease (COPD) is one of the leading causes of human morbidity and mortality globally. Its significant extra pulmonary effects have been well evidenced by many studies by different researchers. Age related macular degeneration (ARMD) which is a very common cause of blindness in elderly people is a common occurrence in many COPD cases in our clinical practice. The present study was attempted to find the existence of age related macular degeneration (ARMD) in elderly COPD patients. The study was conducted in a medical college hospital of Andhra Pradesh which is a tertiary care centre. The study was conducted among 107 COPD patients above 50 years of age. All the patients were subjected to examination of the fundus of their eyes. All statistical analyses were performed by MS Excel 2007. In twenty three subjects evidence of age related macular degeneration was found. The ARMD was more in severe and very severe stage of COPD. It was also observed more in the current smokers, especially those who are smoking more number of cigars per day. Among all the smokers 22.6% were having ARMD. Even the ARMD was also found in 24% of former smokers, those who have already stopped smoking earlier. In two non-smoker COPD subjects also ARMD was detected. The present study attempted to establish a causal relationship between these two disease entities and many significant observations were made.
Keywords: COPD, GOLD Staging, ARMD.
Full Text:
INTRODUCTION
Chronic Obstructive Pulmonary Disease (COPD) is one of the major causes of chronic morbidity and mortality, worldwide. According to the Global Initiative for chronic obstructive lung diseases (GOLD) guideline updated in 2008, COPD is preventable and treatable disease of the lung with some significant extra pulmonary effect that mostly contributes to the severity of the disease 1. There are many significant extra pulmonary effects of COPD. Cardiovascular, mental and musculoskeletal co-morbidities are few in the list. The disease itself leads to decrease in physical activities of the patient and consequently causes systemic inflammation and left cardiac dysfunctions 2. Local and systemic inflammation, oxidative stress, and derangement in the neurohumoral mechanism are some of the probable reasons for development of these extra-pulmonary complications of COPD 3. Patients with COPD are at increased risk of developing cardiovascular diseases, anaemia, cachexia, osteoporosis, peripheral muscle weakness, cognitive dysfunction and many other systemic conditions. These systemic disorders contribute significantly to the morbidity and mortality in COPD patients. In our regular practice it is observed that many elderly COPD patients complains of defective vision. Along with co-morbidities like cataract we could detect age related macular degeneration (ARMD) in many such individuals.
Age Related Macular Degeneration (ARMD) is one of the leading causes of blindness in elderly people. It is characterized by pigmentary disturbances in the macula of retina. There is progressive degeneration of the retinal pigmentary epithelium (RPE), which is located between the retina and the choroid. International epidemiological age related macular study group defines ARMD as a degenerative disorder of the retina in individuals above 50 years of age 4. The pathogenesis of the disease is not clear. Oxidative stress or antioxidant deficiency may be one of the probable causes of ARMD 5. COPD, the disease itself also leads to increase oxidative stress. The activated leucocytes in COPD usually generate oxygen free radicals by induction of enzymes like NAPDH oxidase, superoxide dismutase, nitric oxide synthase and myeloperoxidase6. Rehman et al in a study found that COPD patients experience more oxidative stress in comparison to the control group 7.
In a study by Nadeem et al it was suggested that there is an imbalance between systemic oxidants and anti-oxidants in the COPD patients 8. There is multi-factorial aetiology for the oxidative burden in COPD. Hypoxemia, poor nutrition, inflammation, infection, and smoking have all been attributed. Smoking is a significant risk factor for the ARMD to develop (POLA Study) 9. Many of the patients in our study group were smokers also.
OBJECTIVE
The present study was conducted to establish causal relationship between these two disease entities, with a hypothesis that COPD may be associated with ARMD in elderly individuals.
MATERIALS AND METHODS
All patients above 50 years diagnosed as COPD attending the department of Pulmonary medicine between February 2010 and January 2012 were sent to the Ophthalmology outpatient department for fundus examination. Fundus photograph was taken for those patients in whom relevant ARMD features were found. Patients having associated co-morbidities like diabetes mellitus and hypertension were excluded from the study. Patients having associated cataract and other maculopathies were also excluded from the study.
Out of the total 349 patients only 107 (86 males and 21 females) were made eligible for the study after exclusion. Ethical clearance from the Institutional Ethical Committee was obtained and Informed consent was also taken from all the participants before the study. The diagnosis of COPD was established in all the participants after a thorough clinical history, examinations, chest X-ray and spirometry. Spirometry was performed by computerized Superspiro spirometer in all the participants. Baseline and post bronchodilator spirometry was conducted. The post bronchodilator FEV1 values were taken into consideration for grading the participants as per the staging suggested by the GOLD guideline. The patients were divided into four stages of severity, according to the post-bronchodilator FEV1 values. Mild: FEV1 >80%; Moderate: FEV1 < 80% and > 50%; Severe: FEV1 < 50% and > 30 %; Very severe: FEV1 < 30 %. They were examined for visual acuity using Snellen’s Chart. All the study participants also underwent thorough dilated slit lamp and fundus examination. Those who were having dense cataract, which obstructed fundus examination were excluded from the study. Evidence of ARMD was confirmed during the fundus examination taking the following findings into account.
- Areas of hyperpigmentation
- Areas of depigmentation or hypopigmentation
- Choroidal neovasculaization
- Fibrovascular disciform scarring
Drusens, hyperpigmentation and hypopigmentations are considered as dry ARMD. The size of the drusens was measured with the help of Zeiss fundus camera at 30° and 3X magnification. Findings like Choroidal neovasculaization, Fibrovascular disciform scarring was considered as findings of wet ARMD.
All statistical analyses were performed by Micro Soft Excel 2007. Values were presented as mean ± SD. Variables were expressed as percentages. Chi-square test (fisher’s exact test) was used for examining the qualitative data. For all statistical analyses, p <0.05 was considered statistically significant.
RESULTS
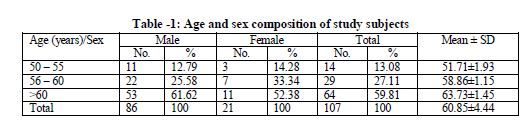
Out of total 107 study subjects majority i.e. 80.37% were male and only 19.63% were female. In our study, 59.81% were above 60 years of age. (Table -1)
All the participants were grouped into four groups according to their severity. Each participant was put under one of the four severity stages according to the GOLD classification 1. In this study group 53 members were current smokers, 37 members were former smokers who had given up smoking earlier and 17 members had never smoked. Almost all the smokers in the study group were habituated to the home made cigars, locally called as chutta. So instead of calculating the smoking index or pack years we classified the smokers according to the number of cigars smoked per day basing on the history given by the study participants. Among the current smokers only two participants were having mild COPD (both males), 21 participants were having moderate COPD (20 males and one female), 18 participants were having severe COPD (14 males and four females) and 12 participants were having very severe COPD (all males). Out of 37 former smokers four persons were having mild COPD (all males), eight were having moderate COPD (six males and two females), 11 were having severe COPD (eight males and three females) and 14 participants were having very severe COPD (nine males and five females). Amongst 17 non smokers 13 participants had mild COPD (11 males, two Females) and four participants (one males and three females) had moderate COPD. None of them had severe or very severe COPD. In our study group we found age related macular degeneration (ARMD) in 23 individuals. There are nine persons with ARMD in each group of severe and very severe stage of COPD patients (Table- 2). The table shows that four severity stages were highly significantly associated with smoking groups.
ARMD was found to be more in the age group of > 60 years (61%) and followed by 56-60 years (22%). This also increases with GOLD severity III & IV (Table 3). In our study group we found age related macular degeneration (ARMD) in 23 individuals. There are nine persons with ARMD in each group of severe and very severe stage of COPD patients. Severity status was significantly varied with age among ARMD study participants.
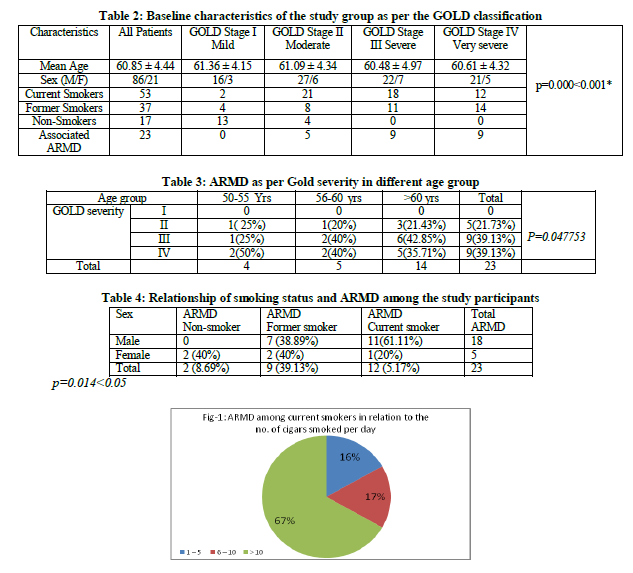
There were 12 ARMD cases among the current smokers group. Even among former smokers we got nine persons having ARMD. Majority among the current smokers (67%) are consuming > 10 cigars /chuttas per day. Smoking status was significantly associated with sex among ARMD study participants.(Table- 4)
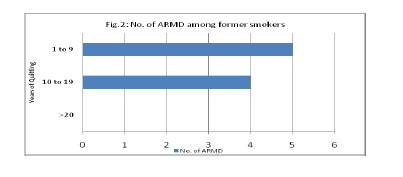
Those who were smoking more than 10 cigars per day were more affected with ARMD (Figure- 1). Among the former smokers it was found that the number of ARMD is more in subjects who quitted smoking recently in comparison to those who quitted long back (Figure- 2). Among the non-smoker COPD patients also we found ARMD in two individuals and both of them are females.
DISCUSSION
The effect of COPD on different organ systems has been studied earlier by different authors. Many authors have confirmed the existence of cardiovascular, skeletal, neuromuscular and psychiatric disturbances as co-morbidities in COPD.2, 7, 10 O. KAYACAN et al in a study detected peripheral neuropathy in COPD patients.11According to study conducted by Murat Sezer et al the visual evoke potential (VEP) of patients with COPD, is altered probably due to hypoxemia caused by ventilation perfusion imbalance in COPD.12 In POLA (Pathologies Oculaires Lie´es a` l’Age) study conducted among 2196 participants it was confirmed that tobacco smoking is a causative agent for the ARMD. In our study we found ARMD in 12 out of 53 smokers. The POLA study also says that former smokers are vulnerable for development of the ARMD too9. In our study group out of the 37 former smokers nine persons were having features of ARMD. Among the former smokers those who had stopped smoking for more than 20 years are not having ARMD but there are good numbers of ARMD cases among recent quitters. Daisy Chan in a review article concluded that there is biologically and statistically plausible relationship between cigarette smoking and ARMD13. Hypoxia, microinfarction and degenerative changes are the contributing factors which are attributed to decreased HDL (High density lipoprotein), increased platelet aggregation and thrombosis in smokers. In our study we also found ARMD in two among 17 non-smoking COPD subjects, that to both of them are females. Though it is statistically not significant we can postulate the association of ARMD in non-smoking COPD cases also.
CONCLUSION
We conclude in this study that age related macular degeneration may be an associated systemic manifestation in elderly COPD patients and particularly among those who are continuing smoking. However a larger multicentric study with a bigger sample size may throw some light in establishing the hypothesis that the ARMD is one of the different co-morbidities in patients with COPD. A routine ophthalmological checkup may be suggested in this context for all COPD patients.
ACKNOWLEDGEMENT
We are grateful to Prof. K.V Ramana Rao for his advice and guidance. We are acknowledging the contribution of Mr. N. Lakshman Rao and Mr.Ganapathy Swamy, our statisticians for helping in statistical calculation. The authors are ever thankful to all the study participants who gave their consent for participating in the study. Authors acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
- KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P,Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007; 176:532–555.
- Henrik Watz, Benjamin Waschki, Corinna Boehme, Martin Claussen, Thorsten Meyer, and Helgo Magnussen. Extrapulmonary Effects of Chronic Obstructive Pulmonary Disease on Physical Activity A Cross-sectional Study American Journal Of Respiratory And Critical Care Medicine Vol 177 2008:743- 751.
- Jan Tkac, S. F. Paul Man, Don D. Sin Systemic consequences of COPD Therapeutic Advances in Respiratory Disease (2007) 1(1) 47–59.
- Stephen j. Ryan; Retina; 4th edition; Volume-2; Page 1041
- Christen WG Jr.; Antioxidants and eye disease Am J Med. 1994 Sep 26;97(3A):14S-17S; discussion 22S-28S.
- Ján Tká?c, S. F. Paul Man, Don D. Sin Systemic consequences of COPD Therapeutic Advances in Respiratory Disease (2007) 1(1) 47–59
- Irfan Rahman, Douglas Morrison, Kenneth Donaldson, And William MAcNEE; Systemic Oxidative Stress in Asthma, COPD, and Smokers AM J RESPIR CRIT CARE MED 1996;154:1055-60
- Nadeem A, Raj HG, Chhabra SK; Increased oxidative stress and altered levels of antioxidants in chronic obstructive pulmonary disease; Inflammation. 2005 Feb;29(1):23-32.
- Smoking and Age-related Macular Degeneration The POLA Study Arch Ophthalmol. 1998; 116:1031-1035
- Joan B. Soriano et al; Patterns of Co morbidities in Newly Diagnosed COPD and Asthma in Primary Care;CHEST 2005; 128:2099–2107.
- O. Kayacan, S. Beder, G. Deda, D. Karnak; Neurophysiological Changes In Copd patients with chronic respiratory insufficiency; Acta neurol. belg., 2001, 101, 160-165
- Sezer Et Al ;Visual Evoked Potential Changes In Chronic Obstructive Pulmonary Disease; Eur J Gen Med 2007;4(3):115-118
- Daisy Chan OD ; Cigarette smoking and age related macular degeneration; Optometry and vision science, Vol. 75, No:7, July 1998; 476 – 48.
Abbreviations
COPD – Chronic Obstructive Pulmonary Disease
GOLD - Global Initiative for chronic obstructive lung diseases
ARMD - Age related macular degeneration
RPE - Retinal pigmentary epithelium
NAPDH - Nicotinamide adenine dinucleotide phosphate (Reduced Form)
FEV1 - Forced Expiratory Volume in one second
SD - Standard Deviation
VEP - Visual Evoke Potential
POLA - Pathologies Oculaires Lie´es a` l’Age
HDL - High density lipoprotein
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License