IJCRR - 5(19), October, 2013
Pages: 132-142
Date of Publication: 19-Oct-2013
Print Article
Download XML Download PDF
DISTRIBUTION OF VAGUS NERVES TO STOMACH AND ITS VARIATIONS
Author: Ch. D. Sukumar, Mahalakshmamma V., Udaya Kumar P., Gajendra (Late)
Category: Healthcare
Abstract:Introduction: It is a well established fact that \"vagotomy\" in varying degrees is a decisively relieving surgical procedure in peptic ulcer patients. Failure of vagotomy or recurrence of paptic ulcer symptoms is due to the variations in the pattern of distribution of the gastric nerves to stomach. Complexity of varying pattern of the gastric nerves supplying the stomach compels a thorough investigation in this context. Materials and Methods: Total of 30 Stomachs with lower part of esophagus and pylorus were utilized for the study from the department of anatomy of Narayana Medical College, Nellore, and Andhra Pradesh. Each specimen was labeled soon after collection and then preserved in a small tank containing 10% formalin. The nerve trunks and their branches were traced by standard dissection methods. Results and Conclusion: In the present study of 30 specimens in 20% of gastric nerves variation were found in its course, pattern and communication; which can produce secretion of acid inspite of conventional vagotomy. It could be suggested that high selective vagotomy can a method of choice for treatment of specific cases of paptic ulcer because of the variations found in the distribution of vagi to the stomach.
Keywords: Stomach, Vagus nerve, Vagotomy.
Full Text:
INTRODUCTION
It is a well established fact that “vagotomy” in varying degrees is a decisively relieving surgical procedure in peptic ulcer patients. However there have been instances of recurrent or persistent pain, which is due to an incompletely sectioned vagus nerve. Complexity of varying pattern of the vagus nerves supplying the stomach and necessity of highly selective vagatomy in specific cases compels a thorough investigation in this context.
NORMAL ANATOMY
Vagal trunks above the level of the diaphragm:
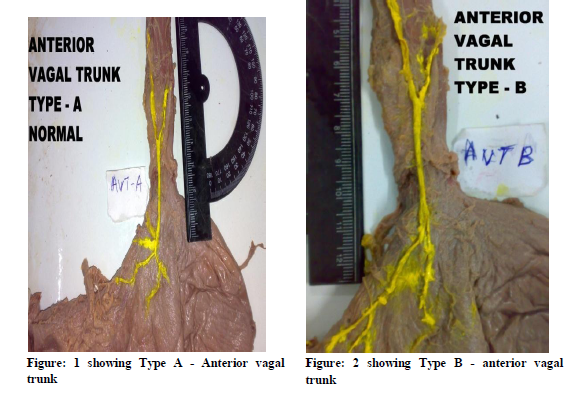
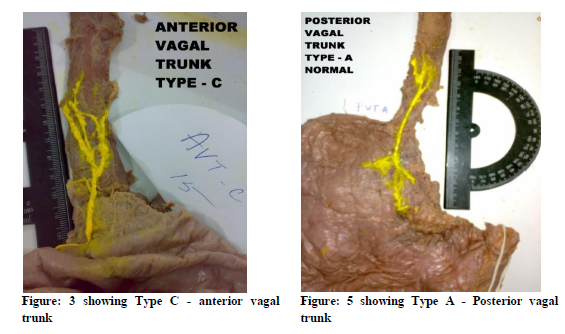
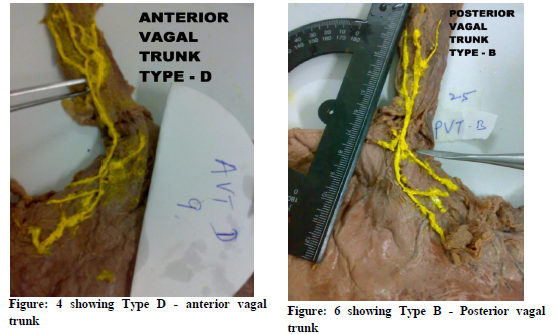
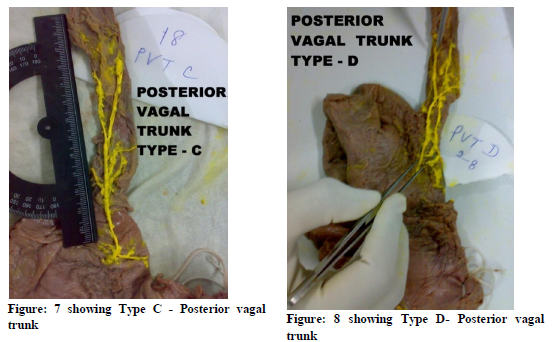
Richard Gentry Jackson8 described four types of anterior and posterior vagal trunks above the level of the diaphragm. In type A, Vagus is single trunk above and below the diaphragm. In type B it becomes a single trunk some distance above the diaphragm but divides into two or more trunks before passing through the esophageal opening of the diaphragm. Vagus becomes a single trunk only at the diaphragm but some distance above the diaphragm it has multiple trunks as in type C whereas it never becomes single trunk at or above the diaphragm in type D
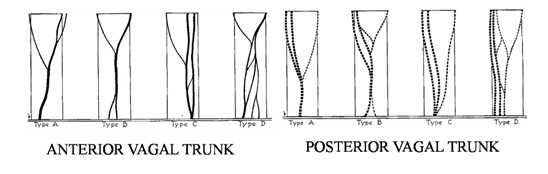
Diagram No. 1 Showing different types of anterior and posterior vagal trunks
Vagal trunks below the level of esophageal opening of the diaphragm
The Anterior vagal trunk passes through the diaphragm and gives off hepatic, gastric, pyloric and celiac branches which supply the liver, biliary apparatus, duodenum, Pancreas, and the pyloric antrum through Celiac plexus or hepatic plexus. The most medial of the gastric branch, which runs parallel to lesser curvature, is known as nerve of the latarjet or principle anterior nerve of lesser curvature.
The posterior vagal trunk gives off hepatic, gastric and celiac branches below the diaphragm. The hepatic branches reach the hepatic plexus either independently or by joining the hepatic branch of anterior vagal trunk. The gastric and coeliac branches of the posterior vagal trunk are same as anterior vagal trunk.
MATERIALS AND METHODS
Total 30 Stomachs, with intact lower part of esophagus and pylorus, were collected for the study from the department of anatomy of Narayana Medical College, Andhra Pradesh. All the specimens collected belonged to cadavers of adult south Indians of unknown profession and food habits.
The collected specimens were labeled and subsequently preserved in 10% formalin. The Specimens had not been subjected to any operative procedures before death. Vagal trunks were traced from lower part of esophageal plexus to the level of the diaphragm carefully. The dissection was continued till the branches of vagal trunks reached the wall of the stomach. Gastric and pyloric branches, Nerves of latarjet, Anterior and posterior vagal trunks with their communications were also traced.
The vagi and its branches were colored and photographed from the lower end of oesophageal plexus. Small thin fibres which were torn during dissection were not seen in the photographs. The length of the vagal trunks was measured from the level of the diaphragm to the lower end of the oesophageal plexus using an ordinary scale. Communicating branches and nerves of latarjet were also observed and measured.
RESULTS
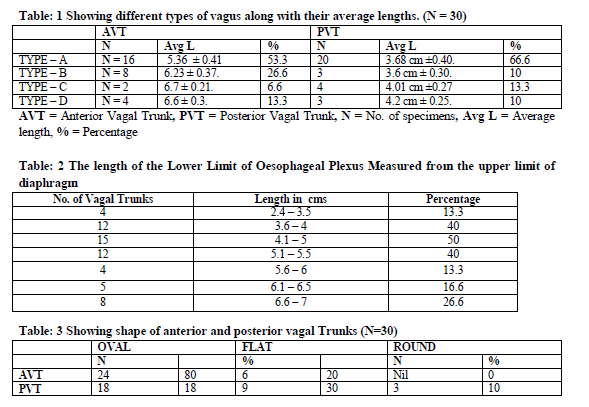
In the present study of 30 specimens, on an average, Type-A (simple pattern) was found in 59.9% and Type-B (intermediate pattern) in 18.3%. Type-C and Type-D were found in 9.9% and 21.6% of the specimens respectively. The average lengths and percentage of AVT and PVT of all types were shown in Table no.1. The length of the lower limit of esophageal Plexus measured from the upper limit of diaphragm are shown in Table no.2.
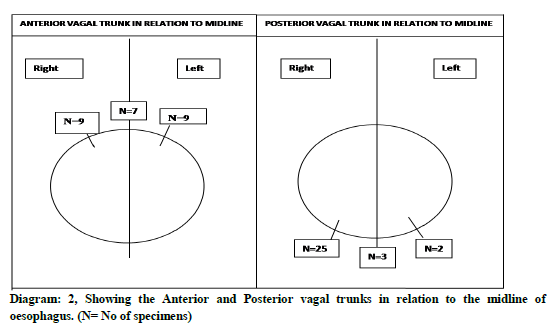
Single trunks were measured for their shape and position which varied with reference to the midline on the esophagus. They are shown in the table no.3 and diagram no.2 respectively.
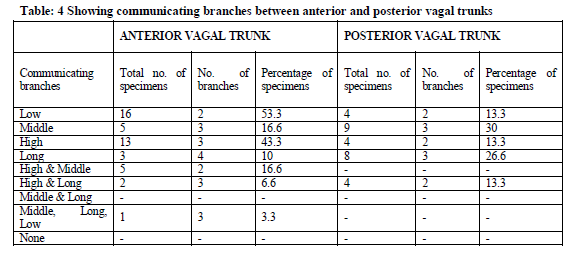
Communicating branches between anterior and posterior vagal trunks were measured and described as low, mid, high and long communicating branches which are shown in table no.4
Variations observed in the branching pattern of anterior vagal trunk:
Normally anterior vagal trunk passes through the diaphragm as a single trunk and gives off gastric, pyloric and celiac and hepatic branches.
In 4 specimens the upper gastric branches arose at or above the level of oesophageal hiatus of the diaphragm. There were no gastric branches in the 3 specimens. The nerve of latarjet was present in 76.6% percent of specimens. In 50% of specimens it was found to communicate with recurrent branch of the hepatogastric nerve. In 2 specimens it divided at its origin about 3 to 4 cms in common with the pyloric nerve. The length of the nerve varied from 2.5 cms to 9 cms.
It was observed that the coeliac branches of the anterior vagus nerve reach the coeliac plexus by at least 3 routes.
-
- Fibres ascended to the coeliac plexus via Hepatic plexus and hepatic artery.
- Fibres joined the sympathetic fibres running along the left gastric artery from pyloric branches.
- Fibres given off directly from the anterior vagus nerves to coeliac plexus.
Pyloric branches of the anterior vagus were present in 8 specimens. In 7 specimens it was from lower hepatic branches or branches of nerve of latarjet.
The hepatic branches were observed to run 1.5 cm to 2.5 cm away from the lesser curvature. Some branches arose in common with pyloric branches. A few hepatic branches arose in common with the nerve of latarjet.
Variations observed in the branching pattern of posterior vagal trunk:
The variations of PVT were seen as follows:
- It was given off above the level of oesophageal hiatus.
- It arose with the nerve of latarjet.
- In 2 specimens there was no clear division and it descended directly to coeliac plexus and numerous fine gastric branches sprang from it.
- In one specimen the main stem descended directly towards the coeliac plexus.
- In one specimen the anterior vagus nerve was thin and the posterior vagus nerve supplied both the surface of the stomach.
The hepatic branches were traced to hepatic plexus via the coeliac plexus and the hepatogastric ligament. In 10 specimens hepatic branches accompanied, the hepatic branches of the left gastric artery. The gastric branches originated at the level of the oesophageal hiatus of the diaphragm or in the thorax. The posterior vagus also gave off extra anterior gastric or hepatic branches. The coeliac branches comprised the major portion of the posterior vagus which formed plexus around the left gastric artery.
DISCUSSION
A large variety of surgical procedures were introduced for the treatment of peptic ulcer. The introduction by dragstedt1, 2 and his associates of the complete division of the vagus nerve supply to the stomach have been accepted as a method of choice. Grimson3 and Moore4 reported that vagotomy was not the final answer to the treatment of peptic ulcer even though in a vast majority of the cases there has been a relief of gastric pain following vagotomy.
1. Pattern of Anterior vagal trunk (AVT) and posterior vagal trunk (PVT) above the diaphragm.
The anatomic description of vagus nerve and their branches between anterior and posterior vagal trunks above the level of diaphragm have been described by Mitchell5, Chamberllein6, Ruckley7, Jackson8, E and D’arcy McCrea20
Mitchell5 observed that there were no constant numbers of trunks above the diaphragm. Kollman, as quoted by E. D’arcy McCrea, observed anterior trunks to be where as posterior trunk to be single. Chamberllein6 classified the vagus nerve into Simple pattern (60%), Intermediate pattern (16%) and Complex pattern (24%). Ruckley7 observed that in about 66.6% of specimens there was a single anterior trunk. In 91.6% cases PVT was single. Jackson8 described 4 types of AVT and PVT as type A, B, C and D and measured the average lengths of the vagal trunks and also observed that a greater proportion of the posterior communicating branches are of the long type than are the anterior branches.
In the present study of 30 specimens: Type-A (simple pattern) was found in 59.9%. Type-B was (intermediate pattern) was found in 18.3%. Type-C was found in 9.9% and Type-D in 21.6%. The average length of Type-A AVT was 5.36 cms and PVT was 3.68 cm. Type-B AVT was 6.23 cm and PVT was 3.6cms. Type-C AVT was 6.7 cm and PVT was 4.1 cm. Type-D AVT was 6.6 cm and PVT was 4.2 cm. 80% of AVT and 76.6% of PVT were single trunks.
Analysis of AVT showed, Type-A in 53.3%, Type-B in 26.6%, Type-C in 6.6% and Type-D in 13.3% of specimens. Analysis of the PVT showed Type-A 66.6%, Type-B 10%, Type-C 13.3% and Type-D in 10% of specimens.
AVT became single farther above the diaphragm when compared to PVT. More AVTs than PVTs divide before passing through the diaphragm. In type-B the AVT was single for a longer distance before dividing, than the PVT. It was noted that not a single posterior vagal trunk measured more than 5 cm in length above the diaphragm.
II. Pattern of Multiple trunks below the diaphragm
Jackson8 observed that, below the diaphragm, multiple trunks of AVT in 15 specimens (30%) and multiple trunks of in PVT in 4 specimens (8%) of out of 50 specimens. Ruckley7 observed multiple trunks of AVT in 3 specimens (25%) out of 12 and PVT in 1 specimen (8.3%). In the present study, the pattern of multiple trunks below the diaphragm was found in 12 (40%) out of 30 specimens in AVT and 6 (20%) out of 30 specimens in PVT.
III. Communicating Branches
According to Mitchell5, there were no constant number of communicating branches between AVT and PVT. Chamberllein6 found that the communicating branches were prominent in 70%, moderately prominent in 16% and obscure in 14%. According to Ruckley7 AVTs and PVTs were linked by number of long and short communicating strands. According to Jackson8 mid communicating branches were more seen posteriorly than anteriorly (40%) and high communicating branches were seen more anteriorly (33.3%) than posteriorly.
In the present study it was observed that communicating branches from posterior to anterior vagus were passing around the oesophagus or through its muscle fibres. Communicating branches were not seen in all dissections. The communicating branches were classified as mentioned in the results (table no.4). Middle and long communicating branches were more from the posterior vagal trunk (30% and 26.6% respectively).
IV. Position of AVT and PVTs on the oesophagus
The distal end of the oesophagus was usually fixed in position. The position of the AVT and PVT were not constant in relation to the distal end of the oesophagus.
Mitchell5 observed the position of AVT and PVT on distal portion of the oesophagus in relation to anterior and posterior aspects respectively. The anterior vagus nerve was found to pass mainly to the posterior aspect of oesophagus and posterior vagus was found to passes to the anterior aspect of oesophagus occasionally. Chamberllein6 observed that the position of the AVT on the oesophagus was normal in 88% and abnormal in 12% of specimens whereas the position of PVT was normal in 82% and abnormal in 18% of specimens. According to Jackson8 66% of AVT were in normal position and 30% were in abnormal position 38% of PVT were in normal position and 29% were in abnormal position. Walters9, 10 in his studies noted that PVT was not always posterior so it was named right gastric nerve and AVT was named as left gastric nerve. In his study of AVT he found that 32% were towards the right side and 62% were towards the left side. On the posterior aspect 44% of PVTs were towards the right side and 18% were on the left side of oesophagus.
In the present study it was found that distal end of the oesophagus was mostly fixed in position. AVTs were closely applied to the oesophagus and slightly to the left of distal esophagus. The PVTs were on the right of the midline and separated from oesophagus by loose areolar tissue. AVTs were in normal position in 84% and in abnormal position in 16%. The PVTs were in normal position in 33.3% and in abnormal position in 66% (Diagram No.1).
Terminal branches of AVT and PVT
Mitchell5 described that the AVT divided into 4 branches gastric, pyloric, hepatic and coeliac below the diaphragm. The nerve of latarjet may be a branch from pyloric or gastric branch of AVT. E. D’Arcy McCrea20 stated that presence of anterior gastric plexus is variable, either may be present or absent. Jackson8 traced the gastric branches, Hepatic branches, pyloric branches and coeliac branches arising at different levels from AVT. PVT gave gastric, hepatic and coeliac as terminal branches. The anterior nerve of laterjet was the continuation of AVT or pyloric branches and posterior nerve of latarjet follows the continuation of coeliac branches or PVT posteriorly. Jackson8 also noted in two cases that there were no gastric branches anteriorly and in those cases gastric branches of PVT supplied the anterior surface of the stomach. In the study reported by waltman walters 9, 10 the AVT and PVT divided into its terminal branches 3 cm below the level of diaphragm. Johnstone11, 12 and Carter13 observed that the AVT gave off hepatic branches at oesophago gastic junction. AVT continued as anterior nerve of Latarjet. The PVT gave off gastric branches and the posterior nerve of latarjet was the continuation of PVT. According to K C Shanthi14, et al, 11 out of 12 cadavers showed branching of nerve of latarjet forming plexus over anterior surface of stomach, except one in which no branching was observed.
In the present study, the AVT gave off four branches, 3 cms below the diaphragm, as hepatic, gastric, pyloric and coeliac branches. These branches were multiple, the numbers varying from 2-5 branches. The most medial of the gastric trunk was the anterior nerve of latarjet. It was parallel to lesser curvature and ended in the antrum and its length varied from 2.5 to 6 cm from pylorus. The anterior nerve of latarjet was present in 76.6% of specimens. There were no gastric branches in three specimens.
Coeliac branches entered the coeliac plexus via the hepatic branches of the coeliac plexus and along with the hepatic artery. Fibres from pyloric branches or from anterior nerve of latarjet were found to run along the left gastric artery to the stomach. Pyloric branches were often hepatic branches or anterior nerve of latarjet.
The PVT gave hepatic, gastric and coeliac branches. The number varied from 2-3 branches. The most medial branch of gastric nerve was the posterior nerve of latarjet. The PVT was thick and in a few specimens it divided into two divisions and then gave off branches.
In the present study there were no gastric branches in 3 specimens. In 4 specimens upper gastric branches arose at or above the level of the oesophageal hiatus or from the posterior nerve of latarjet which was present in 73.3% of specimens. In one specimen AVT was very thin and the posterior vagus also supplied the anterior surface of the stomach.
The variations of the coeliac division of PVT were as follows:
- It arose at or above the oesophageal opening.
- It arose along with the nerve of latarjet.
- In one specimen the main stem descended directly towards the coeliac ganglia or plexus.
SUMMARY
Vagotomy is the usual procedure followed for treatment of peptic ulcer for many years. W.J. Merle Scott15 observed that recurrence of peptic ulcer symptoms after vagotomy can occur in some cases due to variations in distribution of vagus nerve.
In the present study, of 30 specimens, it was concluded that distinct majority of vagal trunks followed a normal pattern. However about more than 20% showed variable patterns of distribution.
In this study AVT divided at higher level when compared to PVT above the diaphragm. No single PVT trunk measured 4.2 cm above the level of the diaphragm but AVT trunks measured 6 cm.
Multiple trunks were present in 43.3% of specimes above the diaphragm and in 40% of specimens below the diaphragm. Therefore 3.3% more multiple trunks were found above the level of diaphragm when compared to multiple trunks below the level of the diaphragm. Multiple trunks were found more from the PVTs above the diaphragm and more from AVTs below the diaphragm. Majority of Type-A vagal trunks present no technical difficulty for vagotomy, whereas in Type- B, C and D surgeon have to search carefully for all the branches and locate the primary trunks then division has to be made, which poses more technical difficulty but failure of which may lead to recurrence of peptic ulcer symptoms.
Long and middle communicating branches between AVT and PVT were found more in number posteriorly rather than anteriorly. High communicating branches were found more anteriorly..
The distal end of the oesophagus was mostly fixed in position. The AVTs are closely applied to the oesophagus and PVTs are separated from oesophagus by loose areolar tissue. Therefore it is easier to palpate PVTs than AVTs. Common location of vagal trunks was found to be within the area just above the diaphragm right of the anterior midline of the oesophagus for AVTs and right of the posterior midline for PVTs. If the vagus nerve were found located outside these areas they were considered as abnormal in position. Abnormal position of AVTs was in 16% and in PVTs 20%. It was noted that AVTs and PVTs were found within a fairly limited area.
It is preferable to divide the AVT above the diaphragm, because it is usually single and is higher than PVT. The PVT could be divided just below the diaphragm because it was found that it does not become single until it reaches the diaphragm.
CONCLUSION
It is difficult to perform complete vagotomy in Type-C and Type-D vagal trunks. In the present study 10% Type-C and 4.9% Type-D were found. Amdrup, Jenson and wilkison16 introduced the highly selective vagotomy(HSV) where the aberrant fibres supplying the stomach were identified and resected. T F Gorey17, et al and Falk GL18, et al, concluded that HSV is a definitive operation in complicated and chronic duodenal ulceration that allows preservation of the pylorus.
The knowledge of the variations of gastric branches of vagus nerve will help the surgeons to perform better. So, it could be concluded that HSV is method of choice for treatment of peptic ulcer in specific patients because of the variations found in the distribution of vagi to the stomach in the present study.
Competing Interests
The authors declare that we have no competing interests
Ethical committee clearance
As the study included only human cadavers, ethical committee clearance was not taken into consideration. Authors will take the responsibility of any further allegations regarding ethical clearance that arise from the study.
ACKNOWLEDGEMENTS
I thank Dr. Vimala (Late) and my colleagues for their precious suggestions and I extend my gratitude to all the scholars / authors / editors / publishers whose articles, journals are reviewed, cited and included in the references of this manuscript.
References:
- Dragstedt L. R. and Associates; Vagotomy for gastroduodenal ulcer, Ann. Surg., 122, 973, 1945.
- Dragstedt, L. R. and Associates; Removal of the vagus innervation of stomach in gastroduodenal ulcer, Ann. Surg., 17, 742, 1945.
- Grimson K. S. and Associates; The effect of transthoracic vagotomy upon functions of stomach and upon the early clinical course of patients with peptic ulcer, South M. J., 39, 460, 1946.
- Moore F.D. and Chapman; Removal of entire vagus system just below the diaphragm for duodenal ulcer, arch surg 1948; 57: 351.
- Mitchell G. A; Gastric surgery and innervation to stomach, J Anat 1940; 75; 50.
- Chamberlin, J. A., and Winship, T; Anatomical variations of the vagus nerves-their significance in vagus neurectomy, Ann. Surg. 22, 1, 1947.
- Ruckley C. V; A study of the variations of abdominal vagi, Br. J. Surgery 1964 Aug; 51:569-73.
- Richard Gentry Jackson, M.D; Anatomy of the vagus nerves in the region of the lower esophagus and the stomach, Departments of Anatomy and Surgery, University of NicAigan, Ann Arbor, Michigan.
- Walters, W.H, A. Neibling, W. F. Bradley, J. T. Small and J. W. Wilson; Gastric neurectomy for gastric and duodenal ulceration. Anatomic and clinical study, Ann. Surg., 126, 1, 1947.
- walters W. H. A, Neibling, W. F. Bradley., Anatomical distribution of vagus nerve at lower end of the oesophagus., Arch surg 1946; 55:400 – 405.
- Johnston and Goginger; innervation of human stomach wall. Quoted by K. Kyosola L. Richard, T. waris, O. Penttila. J anat 1980; 131: 482-490.
- Johnston and Wilkinson; Highly selective vagotomy without a drainage procedure in the treatment of peptic ulcer, Br. J surg 1970; 86: 289.
- Carter D; Vagotomy in modern surgical practice. Br J Surg, 71: 84.
- K. C. Shanthi, Sudahaseshayyan; Branching pattern of anterior nerve of latarjet and its clinical significance., Journal of clinical and diagnostic research 2011Vol- 5(5): 980 – 983
- W.J. Merle Scott and John A. Schilling; a critique on vagatomy. The contemporary use of vagotomy.
- Amdrup, Jenson, wilkison; Highly selective vagotomy. Operative surgery and management. 11 Edn. Edr wright Bristol 1987; 145.
- T. F. Gorey, F. Lennon, and S. J. Heffernan, Highly selective vagotomy in duodenal ulceration and its complications. A 12-year review. Ann Surg. 1984 August; 200(2): 181–184. PMCID: PMC1250442
- Falk GL, Hollinshead JW, Gillett DJ; Highly selective vagotomy in the treatment of complicated duodenal ulcer. Med J Aust. 1990 Jun 4;152(11):574-6
- Gray’s anatomy, The anatomical basis of clinical practice in : gastro intestinal tract, 39th edn, Elsevier Churchill livigstone; 2005: 1150
- E. D’arcy McCrea, The abdominal distribution of vagus nerve, J Anat. 1924 October; 59(Pt 1): 18–40.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License