IJCRR - 5(20), October, 2013
Pages: 94-100
Date of Publication: 02-Nov-2013
Print Article
Download XML Download PDF
UNICYSTIC AMELOBLASTOMA IN 40 YEAR OLD MALE:A RARE CASE REPORT
Author: Gopal Sharma, Deepa Das, Reema Rao, Sameer Zope
Category: Healthcare
Abstract:The ameloblastoma is a true neoplasm of odontogenic epithelium which has been described as persistent, locally invasive tumor having aggressive but benign growth characteristics. Several clinico-radiological and histological types are included in the ameloblastoma. Apart from the most commonly encountered clinico - pathologic models there are few variants, whose biological profile is unknown or not elicited. Unicystic ameloblastoma (UCA) is one of the types which refers to those cystic lesions that show clinical, radiographic, or gross features of a mandibular cyst, but on histological examination show a typical ameloblastous epithelium lining part of the cystic cavity, with or without luminal and/or mural tumor growth. Here we report a case of UA in a 40-year-old male with detailed clinical, radiographical and histopathological features with differential diagnosis and treatment.
Keywords: Multilocular appearance, Non- dentigerous variant, Mural, Unicystic ameloblastoma.
Full Text:
INTRODUCTION
Many benign lesions cause mandibular swellings, whose origin can be, attributed to odontogenic or non-odontogenic causes. The most commonly encountered are ameloblastomas, radicular cysts, dentigerous cysts, odontogenic keratocysts, central giant cell granulomas, fibro-osseous lesions and osteomas.(1) The most common tumor of odontogenic origin is ameloblastoma, which develops from epithelial cellular elements and dental tissues in their various phases of development.(2) The term ameloblastoma was coined by Churchill in 1934. It represents 1% of all oral odontogenic epithelial tumors and 18% of all odontogenic tumors.(3)
As per the WHO system of 2003, ameloblastoma is classified based on differences in biologic behavior, treatment plan and recurrence rate as follows: classic solid / multicystic ameloblastoma, unicystic ameloblastoma, peripheral ameloblastoma, and desmoplastic ameloblastoma, including the so-called hybrid lesions.(3)
Solid or multicystic variants of ameloblastomas are locally aggressive, and recur if inadequately excised. However, unicystic ameloblastoma was identified as a prognostically distinct entity with less aggressive behavior.(4)
More than 80% of all ameloblastomas are solid or multicystic variants, with unicystic ameloblastoma being an important clinicopathologic form of ameloblastoma and occupying the remaining 20% of the cases along with peripheral ameloblastoma. Peripheral tumors are odontogenic tumors, with the histological characteristics of intraosseous ameloblastoma that occur solely in the soft tissues covering the tooth-bearing parts of the jaws. Unicystic tumors include those that have been variously referred to as mural ameloblastomas, luminal ameloblastomas, and ameloblastomas arising in dentigerous cysts (DCs).(2) It is a less aggressive variant and it has a low rate of recurrence, although lesions showing mural invasion are an exception and should be treated more aggressively.(5)
Here we are presenting a case of UCA in a 40-year-old male in left body of the mandible.
CASE REPORT
A 40 year old male had reported to the Department of Oral Medicine, Diagnosis, and Radiology, Y.M.T Dental college and Hospital, Kharghar, Navi Mumbai, Maharashtra, India with a chief complaint of swelling on left side of the face since 4 months. History revealed that the swelling was gradual in onset and slowly increased to the present size with mild, intermittent pain. Swelling was not associated with fever, malaise or any other symptoms. No history of paraesthesia, weight loss or loss of appetite was reported.
Past dental history of the patient revealed surgical extraction of a tooth in lower left side of the jaw 10 years back. Medical, social and family history were not contributory. On general examination, he was moderately built and nourished with normal vital signs.
Clinical examination
A solitary swelling was seen over left side of the face of about 6x4cm size extending antero-posteriorly from symphysis menti to the angle of mandible and supero-inferiorly from corner of the lip to about 1cm below the lower border of mandible. The skin over the swelling was normal without any change in the colour. On palpation, temperature over the swelling was not raised. The swelling was hard in consistency and slightly tender. Single left submandibular lymph node was palpable, about 2x2 cm in size, firm, mobile and slightly tender. (Figure 1)
Intra oral examination revealed a solitary swelling of about 5x2 cm size on lower left buccal vestibule extending antero-posteriorly from mesial of 34 to distal of 38 and obliterating the buccal vestibule in relation with 34, 35, 37, 38 and the edentulous area of 36 with maximum dimension in 36 region. Lingually, the swelling extended in relation with 34, 35, 37, 38 and the edentulous area of 36. The mucosa over the swelling appeared smooth and normal with no sinus tract or any discharge. On palpation, the swelling was bony hard in consistency and tender with fluctuancy elicited in the 36 region.
The teeth in the affected area were immobile and non tender to percussion. 36 was missing, and37 had proximal caries and occlusal facet.(Figure 2)
A provisional diagnosis of benign odontogenic tumor was given on the basis of age and sex of the patient, site, consistency of the swelling and cortical expansion.
The patient was then subjected to following investigations. A complete hemogram was advised which showed all the values to be in the normal range. Electric pulp vitality testing was done for 31, 32, 33, 34, 35, 37 and 38 which revealed all the teeth to be vital. Intra oral periapical radiograph of 36 region shows missing 36 and well defined multilocular radiolucency in the apical region of 33, 34, 35, and 37 along with root resorption. Lateral mandibular occlusal radiograph revealed a multilocular radiolucency extending from the distal aspect of 32 to the distal aspect of 38 with Buccal and lingual cortical expansion. Orthopantamograph (OPG) revealed a large well-defined multilocular radiolucency on the left body of the mandible, extending antero-posteriorly from the mesial of 31 to the mesial of 38; supero-inferiorly from the alveolar crest region to the lower border of mandible. The internal aspect of the lesion is multilocular with large size locules separated by radiopaque septae giving it as typical soap bubble appearance. The lesion is causing resorption of the roots of 33, 34, 35, and 37 and displacement of the inferior alveolar nerve downwards. The inferior border of the mandible is intact. (Figure 3)
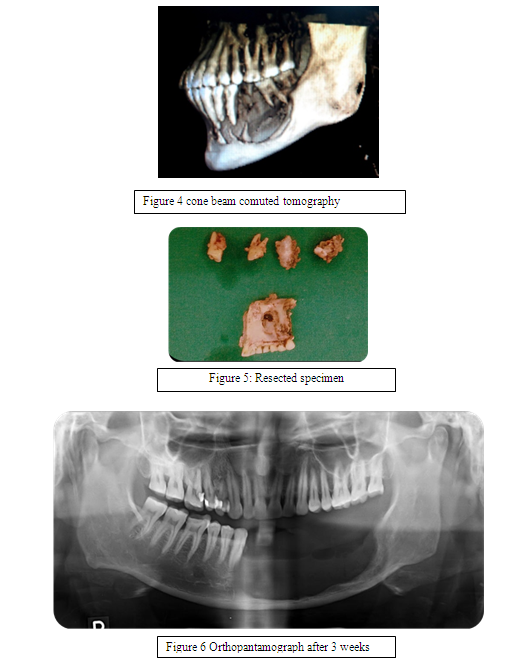
Cone beam computed tomography revealed expansile lesion on the posterior aspect of left side of the mandible, extending antero-posteriorly from the distal of 31 to the distal of 38; supero-inferiorly from the alveolar crest region to the lower border of mandible. The margins of the lesion are well defined. The internal aspect of the lesion is multilocular separated by few septae. Expansion, thinning and discontinuity of the buccal and lingual cortical plates is noted. Thinning and discontinuity of the lower border of mandible is noted along the lingual aspect of 37 and 38 region (Figure 4). The lesion was then aspirated; a thin straw color fluid was obtained from the lesion, which was then sent for the pathological evaluation. The report of it stated as mixed inflammatory lesion.
The differential diagnosis included ameloblastoma, odontogenic keratocyst (OKC), central giant cell granuloma (CGCG), and odontogenic myxoma. Bone biopsy was done. The sample was then sent for the histopathological analysis and a diagnosis of unicystic ameloblastoma is obtained.
En bloc resection of the mandible from mesial of 42 to the distal of 38 was done with peripheral osteotomy sparing the lower border of the mandible. Reconstruction surgery was advised. The post operative specimen measured about 4x5 cm approximately.(Figure 5) The post operative specimen was also subjected for the histopathological analysis and a confirmed diagnosis of unicystic ameloblastoma with mural proliferation was obtained. Post operative OPG after 3 weeks was taken. (Figure 6)
DISCUSSION
Unicystic ameloblastoma, a variant of ameloblastoma, was first described by Robinson and Martinez in 1977. Unicystic ameloblastoma (UCA) is a rare type of ameloblastoma, accounting for about 5-10% of intraosseous ameloblastomas.(6-8) It usually occurs in the second and third decades of life. More than 90% are located in the mandible in the posterior region, followed by the parasymphysis region, the anterior maxilla, and the posterior maxilla(3).
UCA is usually asymptomatic, although a large tumor may cause painless swelling of the jaws with facial asymmetry. This swelling is the result of an expansion of the cortical plates of the jaw and can be identified by palpation as hard and bony.(10) In our case study, patient exhibits slightly tender swelling. The clinical and radiographic findings in most cases of unicystic ameloblastoma suggest that the lesion is an odontogenic cyst, particularly dentigerous cyst. However, few are not associated with impacted teeth which are called non-dentigerous variant. Most of the UCAs are associated with an impacted tooth, the mandibular third molar being involved most often.(1)
The ratio of the maxilla: Mandible is 1:7 for the dentigerous variant, versus 1:4.7 for the non-dentigerous type.(11) Gender distribution shows a slight male predilection with a male: female ratio of 1.6:1 for dentigerous variant. However, when the tumor is not associated with an unerupted tooth, the gender ratio is reversed to a male to female ratio of 1:1.8.(1) In our case, the patient was a male, and the lesion was on the left body of the mandible and a non-dentigerous type.
The pathogenesis of cystic ameloblastomas remains obscure. There have been many debates regarding whether unicystic ameloblastoma develops de novo or arises in an existing cyst. Leider et al, proposed three pathogenic mechanisms for the evolution of Unicystic ameloblastoma: reduced enamel epithelium, from dentigerous cyst and due to cystic degeneration of solid ameloblastoma.(3)
The 2 main radiographic appearance of UCAs has been divided into : unilocular and multilocular, and these have clear preponderance for the unilocular pattern.(5) This preponderance is predominantly marked for the dentigerous variant, where the unilocular to multilocular ratio is 4.3 : 1, and for the nondentigerous type, this ratio is 1.1 : 1 (7). In UCA, involved teeth show varying degrees of root resorption.(12 ) Eversole et al., identified predominant radiographical patterns for UCA: Unilocular, scalloped, macromultilocular, pericoronal, interradicular, or periapical expansile radiolucencies.(11) In this case, the patient was a 40 year old, male and the lesion on radiographs shows multilocular appearance which was not associated with impacted teeth and hence, non-dentigerous type. This makes this case a unique report in the literature of UCA.
The present case was differentiated from other multilocular lesions like solid ameloblastoma, central giant cell granuloma, odontogenic myxoma, and cystic lesions like odontogenic keratocyst (OKC), dentigerous cyst (DC), and residual cyst. Based on fluctuant nature from which gave a positive aspirate, the multilocular lesions like solid ameloblastoma, central giant cell granuloma, odontogenic myxoma was ruled out. OKC produces thick cheesy material instead of thin straw color fluid which is seen in this case. DC is ruled out as there was no impacted tooth present. Residual cyst will not produce so much of expansion as seen in this case.
The early ameloblastic changes within the cyst wall were first described by Vickers and Gorlin in 1970, and their histological criteria for the diagnosis of unicystic ameloblastoma includes a cyst lined by ameloblastic epithelium with a tall columnar basal layer, sub nuclear vacuoles, reverse polarity of hyper chromatic nucleus, and a thin layer of oedematous, degenerating stellate reticulum-like cells on the surface.(13) The mural extension into the cystic wall is the frequently seen feature, and the term mural UCA is used when the thickened lining (either plexiform or follicular) penetrates the adjacent capsular tissue.(12)
In a clinicopathologic study of 57 cases of unicystic ameloblastoma, Ackermann classified this entity into the following three histological groups: (14)
Group I— luminal (tumor confined to the luminal surface of the cyst);
Group II— intraluminal/plexiform (nodular proliferation into the lumen without infiltration of tumor cells into the connective tissue wall);
Group III— mural (invasive islands of ameloblastomatous epithelium in the connective tissue wall not involving the entire epithelium).
Another histologic subgrouping by Philipsen and Reichart has also been described as: (7)
Subgroup 1— luminal;
Subgroup 1.2— luminal and intraluminal;
Subgroup 1.2.3— luminal, intraluminal and intramural;
Subgroup 1.3— luminal and intramural.
The mural variety is seen to be more often associated with the ‘nondentigerous’ type of these lesions, while the intraluminal proliferations are more than twice as frequent in UCAs of the ‘dentigerous’ type.(15)
A definitive diagnosis of unicystic ameloblastoma can only be done by histological examination of the entire lesion and cannot be predicted preoperatively on clinical or radiographic grounds. The epithelial lining of a UCA is not always uniformly characteristic and is often lined partly by a nonspecific thin epithelium that mimics the dentigerous cyst lining. Thus, true nature of the lesion becomes evident only after enucleation when the entire specimen is available for microscopy.(15)
Treatment planning depends on the histological type of UCA. The UCA which is diagnosed as subgroups 1 and 1.2 may be treated conservatively (careful enucleation), whereas Subgroups 1.2.3 and 1.3 should be treated aggressively.(3) As UCA tends to affect young adolescent patients, the concern to minimize surgical trauma and permit jaw function and tooth development to proceed reasonably unimpaired.(15) According to Ackermann et al. classification, this case belongs to Type 3 and the excised specimen was also subjected to histopathological analysis, which confirmed the diagnosis of UCA with mural proliferations.
Whatever surgical approach the surgeon decides to take, long-term follow-up is mandatory as recurrence of unicystic ameloblastoma may be long delayed. However, recent emerging clinical evidence have indicated the aggressive nature of the so-called unicystic ameloblastoma.(17) Lau and Samman reported recurrence rates of 3.6% for resection, 30.5% for enucleation alone, 16% for enucleation followed by Carnoy’s solution application, and 18% by marsupialisation followed by enucleation for UCA.(16)
CONCLUSION
Ameloblastoma is a tumor with a strong propensity of recurrence, especially when the ameloblastic focus penetrates the adjacent tissue from the wall of the cyst. Radiographically, most of ameloblastoma show multilocularity, whereas unicystic ameloblastoma show a single large unilocular radiolucency. Very rarely, we come across a case with presentation of multilocular, non dentigerous variant and unicystic type in the male patient. Unicystic variant of ameloblastoma with aggressive histological behaviour also might be successfully treated with marsupialisation with subsequent enucleation, and this approach should be considered as an alternative to resection.

References:
- Ammanagi R, Keluskar V, Issrani R. Plexiform unicystic ameloblastoma: Report of a case with unusual presentation. Int J Dent Case Reports. 2011; 1: 1–10.
- Ramesh RS, Manjunath S, Ustad TH, Pais S, Shivakumar K. Unicystic ameloblastoma of the mandible: An unusual case report and review of literature. Head Neck Oncol. 2010; 2: 1–5.
- V. Nagalaxmi, Mithare Sangmesh, Kotya Naik Maloth, Srikanth Kodangal,Vani Chappidi, and Stuti Goyal, Unicystic Mural Ameloblastoma: An Unusual Case Report, Hindawi Publishing Corporation Case Reports in Dentistry; Volume 2013.
- Robinson L, Martinez MG. Unicystic ameloblastoma: a prognostically distinct entity. Cancer 1977; 40: 2278–85.
- Gümgüm S, Ho?gören B. Clinical and radiologic behaviour of ameloblastoma in 4 cases. J Can Dent Assoc. 2005; 71: 481–4.
- Reichart PA, Philipsen HP.. Odontogenic tumours and allied lesions. Quintessence Publishing Co UK. 2004: 41-77.
- Leider AS, Eversole LR, Barkin ME. Cystic ameloblastoma: A clinicopathological analysis. Oral Surg Oral Med Oral Pathol 1985; 60: 624-30.
- Gardner DG, Corio RL. Plexiform unicystic ameloblastoma: Variant of ameloblastoma with a low recurrence rate afer enucleation. Cancer 1984; 53: 1730-5.
- Lakshmi Kavitha Nadendla, Unusual imaging appearance of unicystic ameloblastoma. Contemp Clin Dent. 2012 Oct-Dec; 3(4): 475–477.
- Yunus M, Baig N, Haque AU, Aslam A, Atique S, Bostan S, et al. Unicystic ameloblastoma: A distinct clinicopathological entity. Pakistan Oral and Dent J. 2009; 29: 9–12.
- Rastogi S, Nijhawan S, Modi M, Kumar A, Aslam N, Latheef F. A large mixed radiolucent – Radioopaque lesion in the mandible: A nobel diagnostic approach. J Clin Diagn Res. 2010; 4: 2300–7.
- Philipsen, H. P. and Reichart, P. A. Unicystic ameloblastoma. A review of 193 cases from the literature. Oral Oncol. 1998; 34(5): 317-25.
- Braunshtein, E.; Vered, M.; Taicher, S. and Buchner, A. Clear cell odontogenic carcinoma and clear cell ameloblastoma: a single clinicopathologic entity? A new case and comparative analysis of the literature. J. Oral Maxillofac. Surg. 2003; 61(9): 1004-10.
- Ackermann, G. L.; Altini, M. and Shear, M. The unicystic ameloblastoma: a clinicopathological study of 57 cases. J. Oral Pathol. 1998; 17(9-10): 541-6.
- Kiran Kumar, K. R.; Giju Baby George; Sheeba Padiyath and Rupak, S. Mural Unicystic Ameloblastoma Crossing the Midline: A Rare Case Report. Int. J. Odontostomat. 2012; 6(1): 97-103.
- Lau SL, Samman N. Recurrence related to treatment modalities of unicystic ameloblastoma: a systematic review. Int J Oral Maxillofac Surg. 2006; 35: 681–90.
- Li TJ, Kitano M, Arimura K, Sugihara K. Recurrence of unicystic ameloblatoma: A case report and review of the literature. Arch Pathol Lab Med. 1998; 122: 371–4.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License