IJCRR - 5(21), November, 2013
Pages: 83-91
Date of Publication: 21-Nov-2013
Print Article
Download XML Download PDF
DIAGNOSIS OF IRON DEFICIENCY OF CHRONIC KIDNEY DISEASE : VALIDITY OF IRON PARAMETERS, RETICULOCYTE HEMOGLOBIN CONTENT(CHR) AND HYPOCHROMIC RED CELLS IN INFLAMMATORY STATE
Author: Vidyashankar P., Alan F. Almeida, Niwruti K. Hase, Arun Halankar, Harinakshi Rai, Sadanand Bhusari
Category: Healthcare
Abstract:Introduction: Diagnosis of iron deficiency is difficult in presence of uraemia. The validity of these tests in the presence of inflammation has not been studied, and it formed the basis of this enquiry. Methods: On hundred and twenty two consecutive chronic kidney disease (CKD III, IV, V-non dialysis) patients were enrolled. Complete hemogram, iron studies, Reticulocyte hemoglobin content (CHr) and percent hypochromic red cells (%Hypo), high sensitive CRP (hs-CRP) levels were done. In the study group of 122 patients screened, 103 patients were found to be iron deficient by Kidney Dialysis Outcome Quality Initiative (KDOQI) criteria. In the iron deficient patients, intra venous iron (i.v iron sucrose 1000mg) was administered in divided doses followed by erythropoetin and the tests were repeated after 4 weeks of completing i.v iron therapy. If the rise in Hb> 1gm%, at the end of 4 weeks, the patient were grouped into responders (iron deficient subjects). The rest were grouped as non responders(Iron replete).The value of the tests, individually or in combination, was determined in the subgroups and categorized based on hs-CRP levels (< 5mg/L). Results: Fifty eight of the 103 patients responded to i.v iron therapy (iron deficient).Varied sensitivity, specificity, and positive and negative predictive values were noted when tests were used individually or in combination to diagnose iron deficiency anemia. Conclusion: Iron studies are useful screening methods, but In the presence of inflammation, the combination of parameters with CHr and Hypochromic red cells add to specificity.
Keywords: Iron deficiency, iron studies, Reticulocyte hemoglobin content (CHr), Hypochromic red cells (Hypo %), Inflammation.
Full Text:
INTRODUCTION
Diagnosing iron deficiency with currently available tests is rendered difficult in patients with chronic kidney disease due to presence of inflammatory state associated with uremia [1,2,3,4,10]. The accurate diagnosis of iron status is essential in avoiding iron overload, which increases morbidity and mortality. Serum ferritin and transferrin saturation (TSAT) are commonly and easily available tests [12,13,14] for diagnosis. However, serum ferritin is an acute phase reactant, and is raised in the anemia of chronic disease and uremic state, hence these values could be unreliable [3,12,13,33,34].
Newer markers like CHr and hypochromic red cells have been currently introduced to guide iron therapy [18,19,20,26,38,39]. European best practice guidelines 2005 [8,17,27] and K/DOQI 2006 guidelines have recommend these newer parameters, Reticulocyte hemoglobin content (CHr) and Hypochromic red cells (Hypo %) as marker of iron deficiency status. [7,8,9,21,22,23]. But these tests have not been validated in the presence of inflammation ,which is often found in azotemic and hemodialysis patients [11,12,32].
CHr and hypochromic red cells has been shown promising evidence in studies by Fishbane S et al and Cullen P [18,20,22,35,41]. Their validity in inflammatory state have not been evaluated.
There is no single test or in combination have good validity in diagnosis of iron deficiency (34). Hence, poor response to intravenous iron is considered as the gold standard in the diagnosis of iron deficient state (32,33,40,43,50)
SUBJECTS AND METHODS
Patients and study protocol
A Prospective study was conducted at King Edward VII Memorial Hospital affiliated to Seth GS medical college, Mumbai, India. We included 122 (70 males and 52 females) consecutive patients with chronic kidney disease (Stage 3, 4 and 5 not on dialysis) attending the Nephrology outpatient services. Institution ethical committee approval and informed consent were taken before enrollment. Patients with age < 18 years, recent blood transfusions (Preceding 2 months), with active infection, bleeding, malignancy and active liver disease were excluded. After a wash out period of seven days (on oral iron preparation) and for 14 days (on intravenous iron preparation), fasting blood sample was collected and tested for the following parameters . Iron studies including serum iron, TIBC, transferrin saturation and ferritin. Reticulocyte parameters like absolute reticulocyte count (ARC), reticulocyte percentage, corrected reticulocyte index (CRI), reticulocyte hemoglobin content (CHr) and hypochromic red cells (Hypo%). High sensitive C - Reactive Protein (hs-CRP). Blood urea nitrogen, Serum creatinine, Serum electrolytes, urine examination, urine culture, liver function tests. The patients were diagnosed to have iron deficiency if they have one of the following as per Kidney Dialysis Out come Quality Initiative (K/DOQI) criteria (Transferrin saturation (TSAT)< 20 % or Serum ferritin<100 ng/mL) [9,45]. Patients with any one of the above were presumed to have iron deficiency state and were given 1000mg of intravenous iron sucrose to replete the iron stores [8,9,51]. Iron deficient patients were given erythropoietin after repletion of iron stores, initially with the dose of 100 to 150U/kg/week and increments were made accordingly to get maximum response [9].
Red cell parameters, CHr, Hypochromic red cells and iron studies mentioned above was be repeated 4 weeks of completing last dose of iron therapy as applicable .Response to iron was defined as, if they satisfy one of the criteria ( increase in Hemoglobin by ≥1 gm at the end of 4 weeks [20,22,29,40,44,46]. Patients with response intravenous iron were presumed to have iron deficiency state and were taken as a gold standard in comparing various test parameters [32,39,40]. Non responders are those who did not fulfill the above mentioned criteria and were presumed to be iron replete. Patients were grouped into the absence or presence of inflammation based on hsCRP cut off ≤ 5 mg/dl o r> 5 mg/dl respectively [40,43].
Laboratory methods
The samples for the complete blood count, CHr and hypochromic red cells was processed within 3 hrs of collection. The reticulocyte parametres like CHr absolute reticulocyte count, reticulocyte percentage was processed by ADVIA 120 automated hematology analyzer (Bayer’s diagnostics) at Ranbaxy research laboratory [37, 42]. The reticulocytes were stained with RNA stain oxazine 750 and analyzed by flow cytometric principle with proper standardization. Serum ferritin was tested by Enzyme Linked Iimmuno Sorbant Assay technique, iron studies done by colorimetric methods using SESOMEM analyzer. C - Reactive Protein was be measured by immunonephelometric method at the Immunology laboratory department of pathology. Blood urea nitrogen, serum creatinine, serum electrolytes, urine examination, urine culture, liver function tests, viral markers were done at hospital central clinical laboratory.
Statistical analysis
Statistical analysis was performed using the computer software package of social science (SPSS 13.1, 2005: SPSS Inc, IL, USA.) The data was expressed as mean ± Standard Deviation. Comparison of data for responders and non responders were performed by using the t-test or Mann-Whitney U-test as applicable. The inter group comparison was made by analysis of variance test (ANOVA). The sensitivity and specificity, positive and negative predictive values were calculated using appropriate formula. A p value of less ? 0.05 was considered as statistically significant.
RESULTS
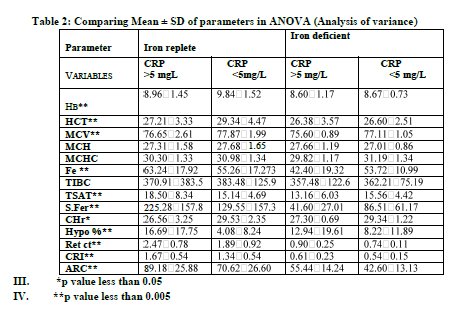
There were 64 males with mean age of 45.32?12.23 years and 39 females with mean age of 41.23?10.34 years were iron deficient. A total of 103 patients were iron-deficient by KDOQI criteria (TSAT < 20% or Serum ferritin <100mg/dl) According to the response criteria mentioned in the study methods,58 (56.31%) patients were iron deficient and 45 (43.68%) were Iron replete as shown in the table 1 and 2.
The base line mean parameters among each sub groups were compared. Parameters like hemoglobin (Hb), TSAT, reticulocyte count (Ret ct), Hypo%, hs CRP (P<0.005), serum iron, TIBC, CHr (P<0.05) were statistically significant among iron deficient and iron replete subjects as shown in table 1.
The sensitivity, specificity, positive and negative predictive values of various tests and their combination is shown in table 3
DISCUSSION
Iron deficiency is the major cause of inadequate response to erythropoeitin therapy in patients with chronic kidney disease. The accurate and early detection of iron deficiency is the most essential step in the management of the patients with chronic kidney disease. However, the diagnosis of iron deficiency in patients with chronic kidney disease is rendered difficult as the currently available tests are less reliable in presence of uremia (inflammatory state) [4, 5]. Measuring reticulocyte hemoglobin content (CHr) and hypochromic red cells (Hypo%) has been proposed as a measure of available iron stores that could be superior to the available tests in various studies[29,30,42,43,47,48].
In this study we specifically investigated for the validity of iron parameters (Serum Ferritin and Transferrin saturation (TSAT), CHr and hypo% in the diagnosis of iron deficiency state in the presence of inflammation. We compared newer parameters with iron studies, and the combination of both parameters taking chosen cut off value of each parameter.In study by Kalantar-Zadeh et al, serum ferritin cut off off < 200ng/ ml had sensitivity of 41 % and specificity of 100 %, TSAT cut off< 20 % had sensitivity of 88 % and specificity of 63 %[14]. In a study by Hesegawa et al (40) found similar predictive power various test parameters as in hemodialysis patients, but the validity of these parameter in the presence of inflammation has not been evaluated . In similar studies by Tessitoire et al[50], in non dialyzed patients, the sensitive of CHr varied from 58.67% to 84.5% and specificity of 78.88 to 88.67%.Validity of theses tests in the presence of inflammation has not been evaluated .
In Hemodialysis patients, a study by Chuang CL et al, had diagnostic sensitivity and specificity of ferritin < 100ng/ml and TSAT < 19 % of 68.6 % and 60.8 % respectively [44]. The efficiency of both tests when used in combination was 64.0 %.When only ferritin <100 mg/ml was taken the diagnostic criteria, sensitivity and specificity was 35.3 % and 78.4 % respectively. The TSAT <19 %, had diagnostic sensitivity and specificity of 58.8 % and 60.8%respectively.
All the above studies had comparable results, but validity of these tests in the presence of inflammation was not shown. Hence in present study it was designed to look for the variation in sensitivity and specificity of iron parameters in the presence of inflammatory state.
In this study, newer parameters like CHr and Hypo% were evaluated in diagnosis of iron deficiency state in non dialysis CKD patients .Their validity was tested in the presence or absence of inflammation.
Studies evaluating the combination of CHr with %hypo with iron studies parameters in predialysis chronic kidney disease patients are very few. In a study by Hesegawa et al (40) found similar predictive power various test parameters as in hemodialysis patients, but the validity of these parameter in the presence of inflammation has not been evaluated .
In similar studies by Tessitoire et al[50], in non dialysis patients, the sensitive of CHr varied from 58.67% to 84.5% and specificity of 78.88 to 88.67%.Validity of theses tests in the presence of inflammation has not been evaluated .
The base line mean MCV, CHr, TSAT, Serum ferritin, Reticulocyte count, were significantly lower in iron deficient in comparison to iron replete subjects. Patients with inflammation had higher mean serum ferritin, low TIBC and Higher %Hypo when compared to absence of inflammation.
CONCLUSIONS
Presence of inflammation interferes with the validity of various tests for the diagnosis. Routine parameters like, iron studies like serum ferritin and TSAT are still useful screening tests with good sensitivity.
Newer parameters like CHr and % Hypo, have variable sensitivity and specificity when used alone in CKD patients. The combination of CHr (<29) and %hypo(>2.5%) with iron parameters like serum ferritin or TSAT increases sensitivity and specificity in presence or absence of inflammation. Serum ferritin alone is a acute phase reactant and has poor specificity in the presence of inflammation. We recommend the tests for diagnosis (iron parameters, CHr, Hypo%) should be correlated with hs CRP(a marker of inflammation) before iron therapy.


References:
- Konijn AM, Hershko C: Anemia of inflammation and Chronic Disease, in iron in immunity, cancer and inflammation, edited by De Souza M, Brock JH, Chechister, John Wiley and sons,:111-143. 1989
- Sears D. Anemia of chronic disease. Med Clin north Am; 76:567-579,1992
- Allan B Schartz, Vinod prasad,Jaslot Garcha.Anemia of chronic Kidney Disease: A combined effect of marginal iron stores and erythropoeitin deficiency. Nephrol Dialysis and Transplantation. Vol 33 No 12, pp 758-767,Dec 2004.
- Sunder-Plausmann G,Horl WH, Spitzauer S .The dilemma of evaluating iron status in dialysis patients-limitations of available diagnostic procedures. Nephrol Dail Transplant; 12:1575-1580,1997
- Navarro JF,Macia ML. Hypochromic red cells as an indicator of iron deficiency. J Rhematol; 24:804-805,1997
- Wittie DL: Can serum ferritin be effectively interpreted in the presence of acute phase response? Clin Chem; 37:484-485,1991
- Dennison HA. Limitation of serum ferritin as a marker of anemia in end stage renal Disease. ANNA J; 26: 409-414,1999
- New European Best Practice for the guideline of anemia of chronic kidney disease. Nephrol Dial Transplantation.20 (7): 1512-1587,2005.
- Clinical practice guideline for management of anemia of chronic kidney disease. K/DOQI update 2006,Am J kid disease 47:855-924, 2006.
- Gokal R,Millard PR, Weatherall DJ, Callender ST et al. Iron metabolism in hemodialysis patients. QJ med; 48:369-391,1979
- Konijn AM, Hershko C.Ferritin synthesis in inflammation: pathogenesis of impaired iron release. Br J Hematol; 37:7-16,1977
- Lipschitz DA,Cook JD,Finch CA;A clinical evaluation of serum ferritin as an index of iron stores.New Eng J Med 290;1213-1216,1974
- Finch CA,Bellotti V,Stray S , Lipschitz DA: Plasma ferritin determination as a diagnostic tool .West Ind J Med 145:657-663,1986
- Kalantar-Zadeh K, Hoffken B, Wunsch H, Fink H, Kleiner M, Luft FC: Diagnosis of iron deficiency anemia in renal failure patients during the post-erythropoietin era. Am J Kidney Dis26 :292– 299,1995
- Rosenberg ME: Role of transferrin measurement in monitoring iron status during recombinant erythropoeitin therapy. Dial Transplant 21:81-90,1992
- Hastika J, Lasserre JJ, Schwatzbeck A, Rieter A, Hehlmann R. Laboratory tests of iron status. Clin Chem., 42:7:712-724. 1996.
- Macdougall IC,Berner CM,Wild BJ,Cavil I et al. Measurement of red cell hypochromasia is a useful indicator of iron status in renal patients. J Am Soc Nephrol; 3:427,1992
- Fishbane S, Galgano C, Langley RC Jr, Canfield W, Maesaka JK. Reticulocyte hemoglobin content in the evaluation of iron status of hemodialysis patients. Kidney Int; 52: 217-22. 1997
- Mittman N, Sreedhara R, Mushnick R, Chattopadhyay J, Zelmanovic D, Vaseghi M, Avram MM. Reticulocyte hemoglobin content predicts functional iron deficiency in hemodialysis patients receiving rHuEPO. Am J Kidney Dis; 30: 912-22. 1997
- Cullen P, Soffker J, Hopfl M, Bremer C, Schlaghecken R, Mehrens T, Assmann G, Schaefer RM. Hypochromic red cells and reticulocyte haemoglobin content as markers of iron-deficient erythropoiesis in patients undergoing chronic haemodialysis. Nephrol Dial Transplant; 14: 659-65. 1999
- Mast AE, Blinder MA, Lu Q, Flax S, Dietzen DJ. Clinical utility of the reticulocyte hemoglobin content in the diagnosis of iron deficiency. Blood; 99: 1489-91.2002
- Fishbane S, Shapiro W, Dutka P, Valenzuela OF, Faubert J. A randomized trial of iron deficiency testing strategies in hemodialysis patients. Kidney Int; 60: 2406-. 2001
- Y. Fukui, S. Samma , K. Fujimoto , A. Yamaguchi , Y. Umeki , M. Ooto, M. Arima Reticulocyte hemoglobin content as a marker of iron status in patients receiving maintenance hemodialysis.J Nephrol ;23:123-135. 2003
- Brugnara C, Chambers LA.Malynn E,Goldberg MA et al. Red blood cell regeneration induced by subcutaneous recombinant erythropoeitin; Iron deficient erythropoeisis in iron replete subjects.Blood;81:956-964,1993
- Mittman N, Sreedhara R, Mushnick R, Chattopadhyay J et al. Reticulocyte hemoglobin content predicts functional iron deficiency in hemodialysis patients receiving erythropoeitin. AM J Kidney Dis; 30:912-922,1997
-
- Brugnara C, Iron deficiency and erythropoeisis .New diagnostic approaches. Clin Chem 49; 1573-1578,2003
- National kidney Foundation .K/DOQI Clinical practice guideline for anemia of chronic kidney disease, Am J Kidney dis; 37:S182-S238, 2001
- Yoshikatsu Kaneko, Shigeru Miyazaki,Yoshihri Hirasawa, Fumitake G et al, Transferrin saturation verses reticulocyte hemoglobin content for iron deficiency in Japanese hemodialysis patients. Kidney Int, 63:1086-1093,2003
- Fishbane S,Galgano C,Langley RC,Canfield W,Mawsaka JK. Reticulocte hemoglobin content in the evaluation of iron status of hemodialysis patients. Kidney Int; 52:217-222,1997
- Brugnara C,Collela GM, Cremins J, Lanmgley RC; Effects of subcutaneous recombinant erythropoeitin in normal subjects. Development of decreased reticulocyte hemoglobin content and iron deficiency erythropoeisis. J lab Clin Med 123:660-667,1994
- Brugnara C,Hipp MJ, Irving PJ, Lathrop H, Lee PA, Minchello EM et al:Automated reticulocyte counting and measurement of reticulocyte cellular indices. Am J Clin Pathol 102:602-632,1994
- Macdougall IC, Caill I, Hulme B, and Bain B et al: Detection of functional iron deficiency during EPO treatment new approach. Br Men J 304:225-226,1992
- Schaefer RM, Schaefer L: The hypochromic red cells: A new parameter fro monitoring of iron supplementation during EPO therapy .J Perinat Med 23:83-88,1995
- Ali MA, Luxtan AW, Walker WHC, Serum ferritin concentration and bone marrow iron studies: a prospective study. Can Med Assoc J; 118:945-946,1978
- Bhandari S, Norfolk D, Brown john A, Turney J. Evaluation of RBC ferritin and reticulocyte measurements in monitoring response to intravenous iron therapy .Am J Kidney Dis; 30:814-821,1997
- Mittman N, Sreedhara R, Mushnik R, et al, Reticulocyte hemoglobin content predicts functional deficiency in hemodialysis patients receiving EPO. Am J Kidney Dis; 30:912-922,1997
- Brugnara C, Zurakowski D, DiCanzio J, Boyd T,Platt O. Reticulocyte hemoglobin content in the diagnosis of iron deficiency in children .JAMA:281:2225-2230,1999
- Brugnara C,Laufer MR, Freidmann AJ, Bridges K, Platt O. Reticulocyte hemoglobin content (CHr):early indicator of iron deficiency and response to therapy,Blood;83:3100-2101,1994
- Tsuchiya K,Saito M,Okano Sugiyama H,Nihei H et al .Monitoring the content of reticulocyte hemoglobin content (CHr) as the progression of anemia in nondialysis CKD patients. Ren Fail; 27; 1:59-65,2005
- Hasegawa M, Kamawara N, Koide S, Murase M et al. Evaluation of reticulocyte hemoglobin content, percentage of hypochronic re blood cells, and ratio of serum ferritin receptor level as a marker of iron deficiency erythropoeisis in patients undergoing hemodialysis. Nephrol Dial Transplant;14;659-665,1999
- Mast AE, Blinder MA, Lu Q, Flax S, Dietzen DJ.Clinical utility of the reticulocyte in the diagnosis of iron deficiency. Blood; 99:1489-91,2002
- Kotisaari S, Romppanen J, Penttila I, Punnonen K.The ADVIA 120 hematology analyzer;red blood cells and reticulocyte indices are useful in the diagnosis of iron deficiency anemia. Euro J Hematology; 68:150-156,2002
- Thomas C, Thomas L. Biochemical markers and hematological indices in the diagnosis of functional iron deficiency. Clin Chem.; 48:1066-1076,2002
-
- Chuang CL, Lui RS,Wei YH, Huang TP et al. Early prediction of response to intravenous iron supplementation by reticulocyte hemoglobin content and high fluorescence reticulocyte count in hemodialysis patients. Nephrol Dial Transplant; 18:370-7,2003.
- Richardson.S ;Optimizing erythropoeitin therapy in hemodialysis patients, Am J Kidney Dis; 38; 1:109-117,2001
- Mitsuki K,Harada A,Miyata Y. The assessment of iron deficiency in chronic hemodialysis patients: investigation of cut off values for reticulocyte hemoglobin content.Clin Exp Nephrol ;7:52-57,2003
- Tsuchiya K, Okano, Teramura M, Iwamoto Y. Content of reticulocyte hemoglobin as a reliable tool for determining iron deficiency in dialysis patients. Clin Nephrol; 59:115-123,2003
- Fukui Y, Samma S, Fujimoto K,Yamaguchi A et al , Reticulocyte hemoglobin content as marker of iron status in patients receiving maintenance hemodialysis. Nippon Suzuki.Jap J of Nephrology,13:124-128,2004
- Macdougall IC, Horl WH, Jacobs C,Vanderrbano F, Parrondo I et al. European best practice guidelines 6-8:assessing and optimizing iron stores .Nephrol Dial Transplant ;15:S20-S32,2000
- Tessitore N, Pietro G,Lippi G,Bassi A et al.The role of iron status markers in predicting response to intravenous iron in hemodialysis patients on maintenance erythropoeitin. Nephrol Dial Transplant; 16:1416-1423,2001
- Silverberg DS, Blum M, Agbaria Z et al; Intravenous iron for treatment of predialysis anemia. Kidney Int; 69:S79-S85, 1999
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License