IJCRR - 5(22), November, 2013
Pages: 74-77
Date of Publication: 04-Dec-2013
Print Article
Download XML Download PDF
BILATERAL HIGH BRANCHING PATTERN OF FEMORAL NERVE - A CLINICO-ANATOMICAL STUDY
Author: Susmita Saha, Rohini Pakhiddey
Category: Healthcare
Abstract:Objective: The aim of reporting this case is to highlight the abnormal or higher branching pattern of the femoral nerve which is very rarely reported. Materials and Methods: The present anomaly was detected during routine course of cadaveric dissection of a 60 year old male cadaver. Result: The present case reports a very early division of the femoral nerve on both sides of the thigh of a 60 years old male cadaver. The femoral nerve descended through the psoas major muscle and divided into two branches; anterior and posterior, 4.1 cm above the midpoint of the inguinal ligament. Conclusion: Knowledge of this kind of variation in the branching pattern of femoral nerve has much academic and clinical value. Furthermore it will be extremely helpful to the surgeons to prevent iatrogenic injury to femoral nerve and for the anaesthetist to give successful block in the femoral nerve.
Keywords: femoral nerve, early division, femoral nerve block
Full Text:
INTRODUCTION
The femoral nerve is the largest branch of the lumbar plexus and it arises from the posterior division of the ventral rami of the second, third and fourth lumber nerves (1.2). The femoral nerve descends on the psoas major muscle and enters the thigh deep to inguinal ligament at the lateral edge of the femoral sheath, which separates it from the femoral artery (2). Conventionally, the femoral nerve is known to divide into anterior and posterior branches below the inguinal ligament (1). This nerve is utilised for nerve block in several surgical procedures and is vulnerable to compression in tight ilio - psoas compartment (3). It may often be injured by sutures or staples, entrapment by tissue scar and local anaesthesia blockade (4, 5). The femoral nerve block is performed on the main trunk of the femoral nerve just below the inguinal ligament (6). The early division of the femoral nerve in the iliac fossa results in incomplete femoral nerve block (3). Prior knowledge of anomalies related to the branching pattern of femoral nerve becomes utmost important for the surgeons while exposing the femoral nerve in the femoral triangle. Hence, it becomes imperative to highlight such an early division of femoral nerve to avoid confusion to surgeons who would usually perform nerve block below the inguinal ligament.
CASE REPORT
During routine dissection of a 60 year old male cadaver in the Department of Anatomy, Maulana Azad Medical College, New Delhi, India, for an undergraduate teaching programme, we detected a higher branching pattern of femoral nerve on both sides of lower limb. The course of the femoral nerve and its relations to other structures were studied carefully and appropriate photography of the variation was done.
The femoral nerve was observed to arise from the posterior division of the ventral rami of the second
to fourth lumber spinal nerves and the nerve was related lateral to the femoral artery. The femoral nerve (‘FN’ in Figure 1) descended along the lateral border of psoas major muscle (‘PM’ in Figure 1) and divided into anterior (‘a’ in Figure 1) and posterior (‘b’ in Figure 1) branches, 4.1 cm above the midpoint of the inguinal ligament (‘IL’ Figure 1). The anterior branches further gave cutaneous branches as well as a branch to the Sartorius (‘s’ in Figure 1) muscle. The posterior branch was located lateral to femoral artery (‘FA’ Figure 1) and was giving saphenous nerve along with branches to the quadriceps muscle. No other abnormalities were noted.
DISCUSSION
The femoral nerve, the psoas major and iliacus muscles are roofed over by the iliacus fascia, which forms a tight fascial compartment. This may account for femoral nerve lesions due to space occupying processes in this area (4). In the cases of femoral nerve paralysis, the existence of some variant muscles or variations in the branching pattern of the femoral nerve may increase the chances of nerve compression (7). The exact knowledge of topographical anatomy of the femoral nerve is required for any successful femoral nerve block. For this procedure, first the inguinal ligament is located, the femoral artery is palpated 2-3 cm below the inguinal ligament and a needle is passed just lateral to the femoral artery (8). Thus, it becomes easy to block the femoral nerve inferior to the inguinal ligament (5, 6). At times, when the femoral nerve has already divided above the inguinal ligament, there are chances that both the branches; the anterior and the posterior branch, may be found deep and inferior to the inguinal ligament (9). Furthermore, any attempt to perform the femoral nerve block may involve incomplete or partial blockage of the divisions of femoral nerve with either of the two branches, i. e. the anterior or the posterior, getting blocked (9). This may be difficult for the orthopaedician and the surgeon who may not be aware of such a fact that the failure of anaesthesia is due to the anomalous early division of the femoral nerve, i. e. branching above the inguinal ligament.
To the best of our knowledge, very few studies have reported such an early division of femoral nerve. Das et al. in 2007 noticed the femoral nerve dividing 3.2 cm above the mid-inguinal point in a male cadaver on both sided of thigh (9). Rajesh et al. have studied the formation and branching pattern of the femoral nerve in sixty four human iliac fossa and observed two lumbar plexuses where femoral nerve was dividing above the inguinal ligament (3). They noticed that in one right lumbar plexus of an adult male cadaver, the nerve divided 4 cm above the inguinal ligament and in another case of a female cadaver; the left femoral nerve divided 3.8cm above the inguinal ligament. In the present case, we observed that the femoral nerve was dividing 4.1 cm above the midpoint of inguinal ligament on both sides of thigh which is at a higher level than previously reported studies. Lack of experience with possible variations could lead to fatal errors in the process of nerve block as well as can cause severe complications during surgical procedures. Variations of such kind could be of assistance to the anaesthetists and surgeons, who go by the conventional knowledge of anatomy regarding the exact site for performing femoral nerve block. To the best of our knowledge, such a very early division of femoral nerve is not documented in previous literature. Awareness of such early division of femoral nerve has much academic and clinical importance.
CONCLUSIONS
Since variations in the branching pattern of femoral nerve are known, it becomes imperative for the anaesthetists and surgeons to be aware of the reported variation in the branching pattern of the femoral nerve while performing femoral nerve block and operating on the lower limbs. Knowledge of this kind of variation will help the
clinicians in preventing iatrogenic complications and for having successful outcome of the surgery.
ACKNOWLEDGEMENT
We would thank our institution for allowing us to dissect cadaver and faculty members without whom this manuscript has been a distant reality.
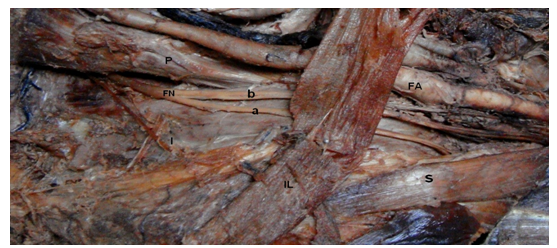
Figure1. Anterior view of the right lower limb showing: FN – Femoral nerve; a – anterior division of femoral nerve (supplying the Sartorius muscle); b – posterior division of femoral nerve; S – Sartorius muscle; FA- Femoral artery; P – Psoas major muscle; IL – Inguinal ligament. Femoral nerve is dividing into anterior and posterior division above the inguinal ligament. Posterior division (b) of the femoral nerve is lateral to the femoral artery (FA)
Figure legends
FN- femoral nerve
- Anterior division of femoral nerve
- Posterior division of femoral nerve
S- Sartorius
FA- femoral artery
P-psoas major muscle
IL-inguinal ligament
References:
- Sinnatamby CS (2001). Last’s Anatomy. Regional and Applied. London: Churchill Livingstone, 2001: pp 115.
- Standring S (2005). Gray’s Anatomy. The Anatomical basisof clinical practice. 38th ed. New York. Elsevier Churchill Livingstone, pp- 1403, 1413 and 1455.
- Rajesh BA, Dave UH. Anatomical variations in formation and branching pattern of the femoral nerve in iliac fossa: A study in 64 human lumber plexuses. People’s Journal of Scientific Research 2011; vol. 4 (2): 14- 19.
- Gracia- Urena MA, Vega V, Rubio G, Velasco MA. The femoral nerve in the repair of inguinal hernia: well worth remembering. Hernia 2005; 9: 348- 7.
- Kim DH, Murovic JA, Tiel RL, Kline DG. Intrapelvic and thigh - level femoral nerve lesions. Management and outcome of 119 surgically treated cases. J Neurosurg 2004; 100:989- 96.
- Ellis H, Feldman S, Harrop G W (2004). Anatomy for anaesthetists. Massachusetts, Blackwell Publishing, 2004: pp- 188-19.
- Warfel BS, Marini SG, Lachmann EA, Nagler W. Delayed femoral nerve palsy following femoral vessel catheterization. Archives of Physical Medicine and Rehabilitation, 1993; 74 (11): 1211-1215.
- Collin VJ. Principles of Anesthesiology.General and regional Anaesthesia. 3rd ed. Pennsylvania: Lea andFebiger, 1993: pp- 1395- 97.
- Das S, Vasudeva N. Anomalous higher branching pattern of the femoral nerve: A case report with clinical implications. Acta Medica 2007; 50 (4): 245- 246.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License